Introduction
Acute appendicitis makes up 30% of the causes of emergency consultations for abdominal pain in pediatric patients (1). Early identification, timely surgical management and prompt hospital discharge by reducing associated complications are the main purposes of comprehensive management of patients with surgical abdominal pathology (2). Acute appendicitis is one of the four major causes why antibiotics are given to hospitalized pediatric patients (3,4), and the first cause of emergency abdominal surgery in pediatrics. In view of this, it is essential to know the clinical and paraclinical characteristics of the care of patients with acute appendicitis, in order to identify opportunities for improvement in the management of this pathology.
During the past five years, the Hospital Universitario San Ignacio (HUSI) has seen changes in surgical techniques, in the complexity of the patients treated and in the strengthening of the surgical and pediatric team. This is why it is important to know the local epidemiology of this condition, the clinical characteristics of the patients, the intraoperative findings and the institutional postoperative evolution and complications (5).
Going deeper into this field will enable an optimization of the care of this type of patients, taking into account that acute appendicitis is the main reason for surgical consultation in pediatric patients, and that we are facing the quality demand as an accredited institution.
Material and methods
We conducted a retrospective descriptive observational study of a cohort of patients diagnosed with acute appendicitis at the HUSI between January 2014 and May 2019. The study included patients between one month and 16 years of age, with clinical or imaging diagnosis undergoing surgery by the pediatric surgery group. We excluded patients who received medical (non-surgical) treatment, patients undergoing general surgery, as well as neonates and patients undergoing extra-institutional surgery referred for further post-operative management.
Through the HUSI Statistics Department, with the DI-SEARCH tool, the authors identified patients diagnosed with acute appendicitis and those undergoing open and laparoscopic appendectomy procedures. The entire list obtained was reviewed. The information of interest was standardized in an Excel format, according to defined variables. A quality control of the data was performed by verifying them by year of collection, as well as a data post-audit and cleansing.
We took into account sociodemographic and clinical variables, as well as clinical care variables; also intraoperative, pathology and culture (germ and sensitivity) findings, complications and paraclinical variables. We analyzed the data statistically using Stata 14, based on the calculation of absolute frequencies and percentages for qualitative variables, as well as mean and standard deviation for quantitative variables.
Results
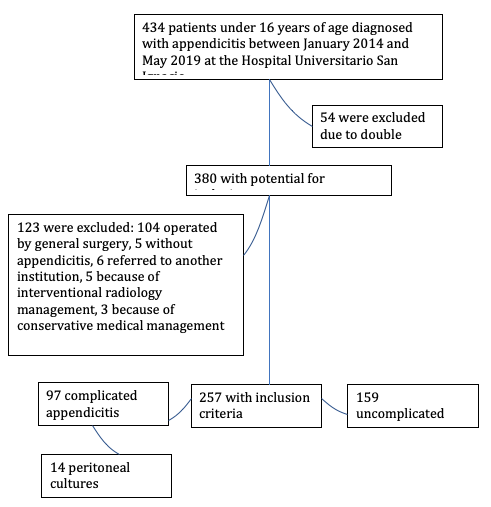
We found 434 records of patients diagnosed with acute appendicitis aged from one month to 16 years, managed at the HUSI. We excluded 54 patients that the program had identified twice, and 123 for other reasons: 5 without appendicitis, 104 operated by general surgery, 6 referred to other institutions to complete the management, 5 managed by interventional radiology, and 3 who did not undergo surgery. We finally obtained 257 records that met the inclusion criteria (Figure 1).
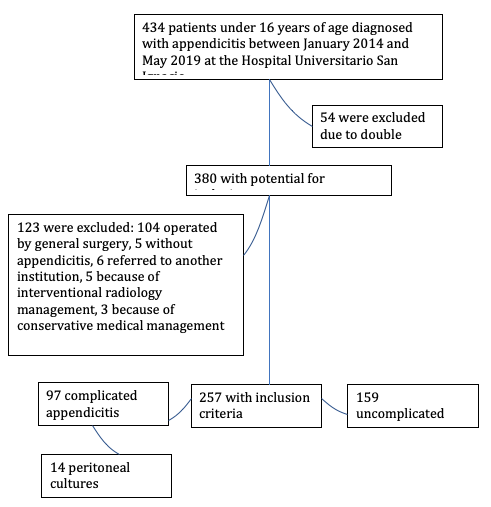 Figure 1.
Flow chart of included and excluded patients
Figure 1.
Flow chart of included and excluded patients
Sociodemographic characteristics
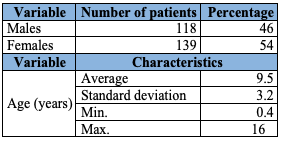
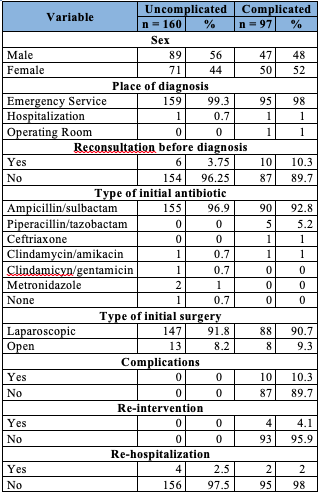
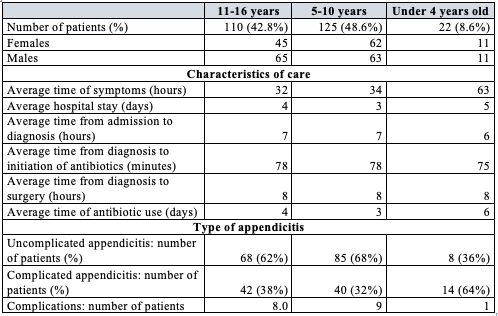
Of the 257 patients included, 118 (46%) were female and 139 (54%) were male, with a mean age of 9.5 years (standard deviation ±3.2 with extreme ages of 4 months to 16 years (Table 1). As for the age subgroups, 8.6% were under 4 years old, 48.6% were between 5 and 10 years old, and 42.8% were between 11 and 16 years old (Table 2).
Table 1 .
Demographic characteristics of patients with acute appendicitis
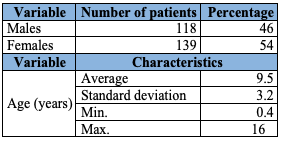
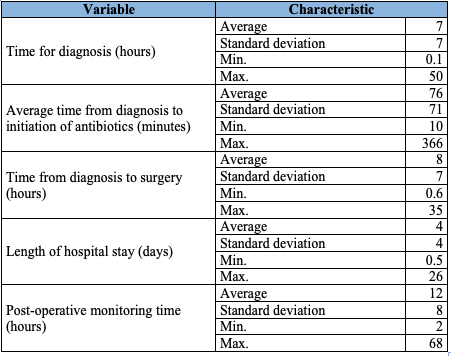
Table 2.
Clinical and care characteristics by age subgroups in acute appendicitis patients
As for the social security of the patients included, 10 (3.2%) of them belonged to the subsidized regime, and the rest to the contributory regime.
Characteristics of clinical care
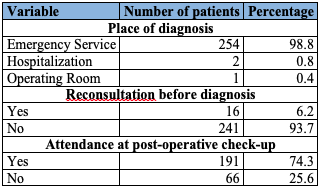
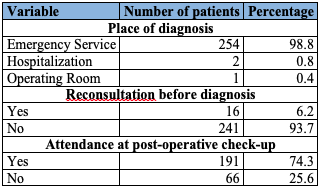
The diagnosis was made in the emergency department of the institution in 98.8% of cases, and the remaining 1.2% were diagnosed in the pediatric hospitalization service. The diagnosis made by the pediatrician or pediatric surgeon was primarily clinical, based on medical record (characteristics of abdominal pain, time of evolution, presence or absence of fever, hyporexia), physical examination (presence or absence of tachycardia, signs of dehydration, Blumberg’s sign, psoas sign, Rovsing’s sign, talopercussion) and paraclinical tests (hemogram, globular sedimentation rate and C-reactive protein); in cases of diagnostic doubt with clinical and paraclinical findings, the diagnosis was confirmed with images such as abdominal ultrasound and CT scan with contrast.
Six percent of the patients had previously consulted the HUSI and had been discharged without a diagnosis of acute appendicitis.
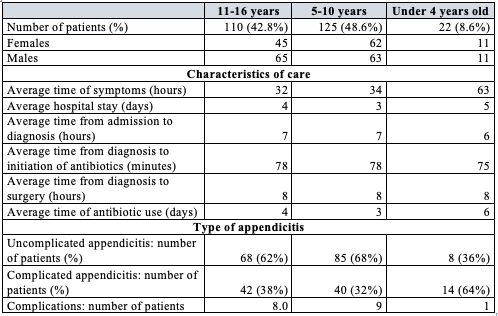
The average time for identification of the disease was 7 hours from admission, and in 57% of the cases identification was achieved within 1 to 6 hours. The average time from diagnosis to the start of antibiotic treatment was 76 minutes, and more than 50% of patients received their first dose of antibiotic within the first hour after diagnosis (Table 3).
Table 3.
Hospital care times for patients with acute appendicitis
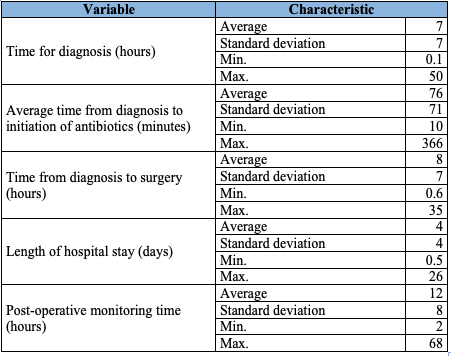
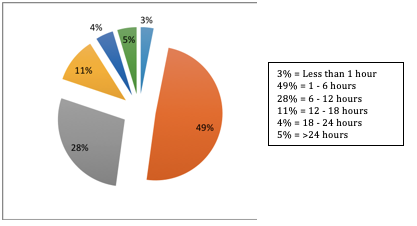
Once the diagnosis was made, the average time until surgery was 8 hours. Most (51%) of the patients had an appendectomy in the first 6 hours after the diagnosis of appendicitis (Figure 2). The average hospital stay was 4 days. The hospital stay of patients with edematous appendicitis was less than 24 hours, and they were discharged in the immediate post-operative period. The maximum reported stay was 26 days in a patient with an intra-abdominal abscess that required re-intervention and management with second-line antibiotics (Table 3).
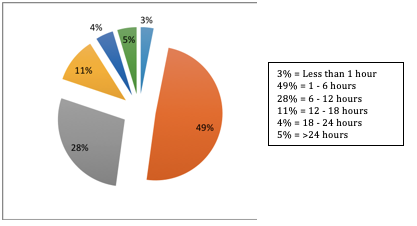 Figure 2 .
Distribution of patients according to the time of appendectomy after diagnosis
Figure 2 .
Distribution of patients according to the time of appendectomy after diagnosis
The average hospital stay was longer in complicated appendicitis, as well as in the under-4 age group, which was 5 days, compared to 3 days in the 11-16 age group (Table 2). In relation to postoperative control after discharge, 74.4% of patients were seen in outpatient follow-up (Table 4).
Table 4.
Characteristics of hospital care
Clinical and paraclinical characteristics
In most cases, the diagnosis of acute appendicitis was based on medical history data and physical examination findings. The average time of symptom evolution at the time of consultation was 36 hours (standard deviation: ±37). Patients under 4 years old had an average time of symptom evolution of 63 hours, compared to 34 and 32 hours for the 5-10 and 11-16 age groups, respectively (Table 2).
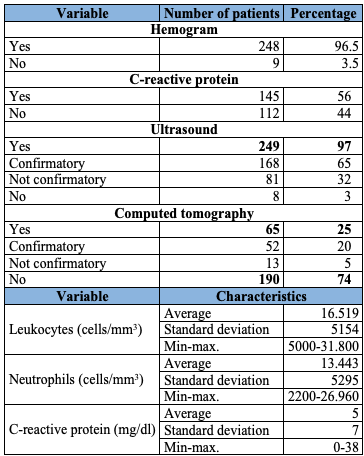
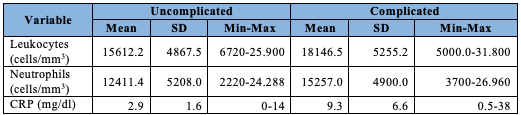
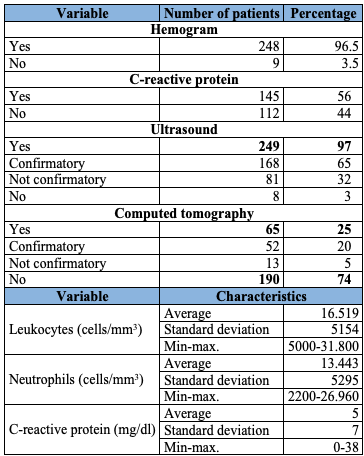
Among the paraclinical tests requested as part of the diagnosis, 96.5% of the patients had a hemogram and globular sedimentation rate, and 56% C-reactive protein. As for hemogram findings, the average leukocyte count was 16,519 cells/mm3, and the average absolute neutrophil count was 13,443 cells/mm3, which showed the tendency to leukocytosis and neutrophilia in the records reviewed. The average C-reactive protein value was 5 mg/dl (standard deviation: ±7). The value of the latter in the complicated appendicitis group was 3 times higher than that of the uncomplicated appendicitis group (Table 5).
Table 5.
Comparison of clinical and paraclinical characteristics between complicated and uncomplicated appendicitis
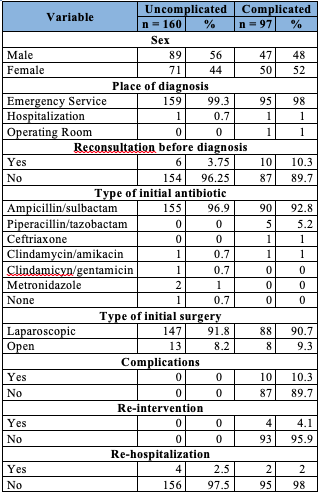
n:number of patients.
Ninety-seven percent of patients had an abdominal ultrasound scan, which was confirmatory and conclusive for appendicitis in 65% of cases. Abdominal tomography was indicated in 25% of patients, in most cases because of persistent diagnostic doubt after abdominal ultrasound. In 20% of the records reviewed, the diagnosis was confirmed by tomography (Table 6).
Table 6.
Paraclinical characteristics of patients with acute appendicitis
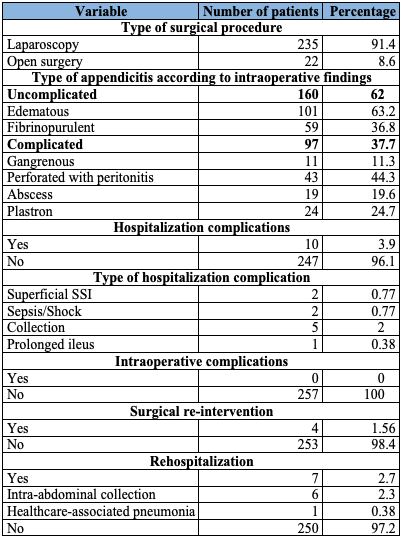
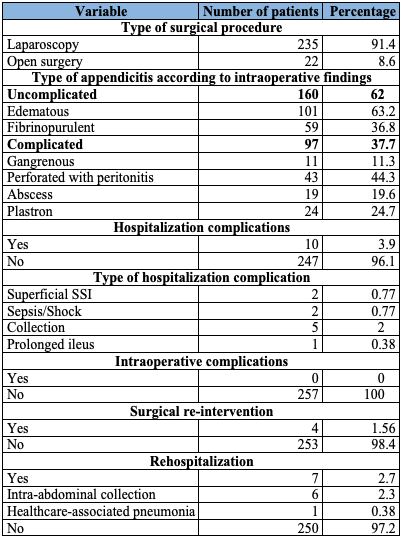
Surgery and surgical findings
Laparoscopic appendectomy was the type of surgery performed most frequently. Surgical findings showed that most cases were of uncomplicated appendicitis (62.3% of patients). The most frequent were edematous appendicitis (63.2%), followed by fibrinopurulent appendicitis (36.8%). As for complicated appendicitis (37.7% of patients), 44.3% were perforated appendicitis with peritonitis, 24.8% appendicular plastron, 19.6% appendicitis with abscess, and 11.3% gangrenous appendicitis (Table 7).
Table 7.
Clinical characteristics and complications in patients with acute appendicitis
Regarding age and intraoperative findings, the average age of presentation of patients with uncomplicated appendicitis was 9.8 years (standard deviation: ±2.9), similar to the complicated appendicitis group, which was 9.2 years (standard deviation: ±3.7). However, it should be noted that in the group of patients under 4 years, 64% were complicated appendicitis, compared to 38% in the 5-10 year age group (Table 2).
The time of symptom evolution in relation to intraoperative findings was longer in the group of patients with complicated appendicitis, with an average of 47.7 hours, while in the uncomplicated appendicitis group it was 31.8 hours (Table 5).
Complications
Complications occurred during hospitalization in 3.9% of patients, but no intraoperative complications were documented. The most common complication was the formation of collections, which occurred in 2% (5 patients) of the cases analyzed and which required re-intervention in four patients, one of which was operated on by interventional radiology and the others by pediatric surgery. Additionally, the following complications were documented: superficial surgical site infection (0.8%), sepsis and shock (0.8%) and prolonged ileus (0.4%).
In 35% of the cases with complications, it was necessary to use a broader-spectrum antimicrobial therapy. Of these, the most frequently used second-line antibiotic was piperacillin/tazobactam in 82% of cases, followed by ertapenem in 14.7% and meropenem in 3.3% of cases (Table 8).
Table 8.
Comparison of paraclinical characteristics between complicated and uncomplicated appendicitis
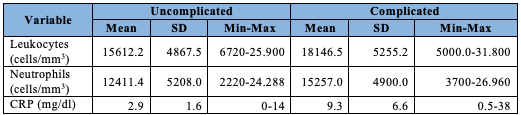
SD:standard deviation
CRP:C-reactive protein
The re-hospitalization rate corresponded to 2.7% of the patients analyzed, mainly for intra-abdominal collections, and one patient for healthcare-associated pneumonia (Table 7).
Microbiological findings
In a first surgical time, peritoneal fluid cultures were taken from 14 (5.4%) patients. One of the cultures tested negative. Thirteen cultures tested positive. Escherichia coli was isolated in 85% of them; there was a phenotype sensitive to all beta-lactams in 72% of the analyses, an extended-spectrum-beta-lactamase resistance pattern in 18%, and an AMPc resistance pattern in 9%. Other microorganisms isolated were Staphylococcus spp. (n = 1), Peptostreptococcus spp. (n = 2), Pseudomonas spp. (n = 1), Bacteroides spp. (n = 1) and Enterococcus spp. (n = 1).
In the surgical re-intervention (indicated by abscess formation), 3 cultures were taken, 2 of which were positive: one for extended-spectrum-beta-lactamase E. coli and one for beta-lactam-sensitive phenotype E. coli. Only one germ was isolated from each culture.
Antibiotic treatment
In relation to the empirical antibiotic treatment initiated after confirmation of the diagnosis, ampicillin/sulbactam was administered more frequently, to 95.3% of patients. In 14% of the minors, it was necessary to change the antimicrobial treatment, because complicated appendicitis or complications were found. Tazobactam/piperacillin was the most widely used second-line antibiotic.
Patients received an average of 70 hours of antimicrobial treatment, with a minimum of 0 hours (in cases where only one preoperative prophylactic dose was administered) and a maximum of 639 hours, in a patient who presented with complicated appendicitis (Table 8). Total antibiotic therapy time was longer for complicated appendicitis, averaging 155 hours; for uncomplicated appendicitis, the average was 20 hours (Table 5).
Discussion
The case series presented here is the first description of pediatric patients with acute appendicitis at the HUSI, and one of the few case series published in Colombia and Latin America. One limitation identified by the authors is that, since the information was obtained from medical records through retrospective review, there were restrictions when collecting the information. Furthermore, the study was carried out in only one institution, which may not be extrapolated to other institutions.
In terms of clinical and care-related characteristics, there were more male patients, similar to what other series have published, with an average age between 9 and 10 years, a little earlier age than that described in the literature (6,7).
From a clinical care point of view, most patients treated at the HUSI were diagnosed by the pediatric and pediatric surgery group in the emergency department, using clinical, paraclinical and imaging criteria. It should be noted that only 6% of the patients had a previous consultation for this condition, without the diagnosis being made. This could be due to the difficulties inherent in diagnosis in this age range, given the presence of non-specific symptoms and clinical characteristics similar to those of other non-surgical pathologies.
An analysis by age subgroups shows that the time of symptom evolution prior to diagnosis was approximately twice as long in the group of those under 4 years, compared to those over 5 years. The difficulty in making the diagnosis may be due to the presence of less clear-cut signs and symptoms; moreover, the time before consultation was also longer. However, in this study there were no differences between age subgroups in the time from admission to diagnosis or the time from diagnosis to surgical procedure. It is noteworthy that more time elapsed before the start of antibiotic treatment in children under 4 years, which could be due to the difficulty in recognizing appendicitis.
In the present study, the average number of leukocytes in the initial hemogram was high for the age ranges, which would suggest the usefulness of scales such as the pediatric score (PAS) (8) in our environment. The criteria of these scales indicate that a leukocyte count greater than 10,000 cells/mm3 may increase the diagnostic probability of appendicitis (8,9). C-reactive protein was tested in just over half the population. In several studies, this biomarker is considered a high-grade diagnostic predictor for complicated appendicitis (9), which coincides with the findings in the population studied, where the C-reactive protein value was higher in complicated appendicitis than in uncomplicated ones. Therefore, C-reactive protein is a useful paraclinical test as a diagnostic predictor of complicated appendicitis.
With regard to the diagnostic images used, it should be noted that computerized axial tomography was indicated less frequently than described in the literature, which could be considered beneficial for patients, due to less exposure to radiation (5).
The drug of choice for empirical management may vary according to institutional protocols and local microbiology (4). The most widely used antibiotic at the HUSI was ampicillin/sulbactam, with a low rate of complications, re-interventions and re-hospitalizations, and with no mortality. These findings may suggest that ampicillin/sulbactam is an excellent alternative for first line empirical management, avoiding the use of broader-spectrum antibiotics, which influence the decrease of antibiotic resistance (10-12).
With respect to the classification of appendicitis, the percentage of complicated appendicitis corresponded to 37.7% of cases. Other published series report complicated appendicitis in 21.5% of patients (13). The rate of appendicular perforation varies between 5 and 62% in the literature, according to the population studied (13,14). The present study showed a perforation rate of 44.3%. The average time of symptom evolution in patients with complicated appendicitis was 47.7 hours, longer than in patients with uncomplicated appendicitis. This is consistent with other authors, who state that more than 60% of patients with complicated appendicitis have symptoms of more than 72 hours of evolution (8,15).
Few peritoneal fluid cultures were performed, and this was one of the limitations of our study, since bacterial isolation is not routinely performed in acute appendicitis. This is in accordance with the recommendations of the American Society for Infectious Diseases, which indicate culture for epidemiological purposes only, to determine local microbiological patterns and optimize antibiotic treatment (14,16). The cultures performed were for aerobic germs, which is also presented in other studies published to date, since anaerobic germ cultures are more difficult and expensive (4,16).
Only 8.2% of patients with complicated appendicitis were handled with open surgery, in line with the literature, which has established that laparoscopic approach is the initial procedure of choice in patients with appendicitis (13,17). For about five years, there have been changes in surgical techniques at the HUSI, and the surgical and pediatric team has been strengthened, so that the laparoscopic approach has become the technique of choice. This is reflected in the low percentage of intra-operative and post-operative complications, as well as in the reduction of hospital stay times.
Conclusions
The management of acute appendicitis in pediatric patients at HUSI reflects the continuous work of the surgical and pediatric team, which has been strengthened in recent years and reflects a clinical care with quality standards at the level of an accredited institution.
Measurement of diagnostic and therapeutic care, such as the time of recognition of the disease, the time to surgery, and the administration of antibiotic therapy, indicate that clinical and surgical care of patients with acute appendicitis is carried out in a manner similar to that reported in the literature.
Among the management characteristics, the success of ampicillin/sulbactam is highlighted, given the low rate of complications. It was also evident that the fact of performing peritoneal fluid cultures did not generate changes in the medical or surgical management, or changes in the short and medium term outcomes.
These data suggest that a reasonable use of resources is feasible, providing high quality care with optimal outcomes and lower cost to the health system.