Introduction
The progressive increase in life expectancy is accompanied by an increase in the incidence and prevalence of chronic non-communicable diseases, and within these, major neurocognitive disorders, characterized by one or more of the following symptoms: decline in cognitive functions, mainly memory, behavioral alteration, and interference with activities of daily living and independence (1).
According to data from the World Health Organization (WHO), in 2019, there were 55 247 million people affected by major neurocognitive disorders worldwide and it is estimated that there will be 785 million by 2030 (2). Based on these data, WHO affirms that major neurocognitive disorders are a public health priority and has formulated a global action plan to be developed between 2017 and 2025, in which it proposes to offer treatment and rehabilitation services that are guided by person-centered care (3).
Since 2011, the Centro de Memoria y Cognición Intellectus has been providing multimodal treatment for older adults with neurocognitive disorders and their families in the Day Hospital service. The model of care is centered on the patient and his or her family (Figure 1). The intervention includes a cognitive stimulation program based on various strategies, including music therapy (4), reminiscence (5), reorientation to reality, cognitive training (6), as well as clinical follow-up, and psychoeducation for the family.
 Figure 1
Multimodal intervention at the Centro de Memoria y Cognición Intellectus
Figure 1
Multimodal intervention at the Centro de Memoria y Cognición Intellectus
Non-pharmacological therapies are known to be useful tools and have few side effects. They have proven to be effective in the treatment of some symptoms, with comparable outcomes in some clinical trials and results equivalent to pharmacological treatments for the improvement of attention, memory, anxiety, and depression, as well as the quality of life of patients (7).
This article aims to present the results of the follow-up of patients who received our intervention for one year, concerning their cognitive and physical functions and their quality of life. At present, there is little evidence available about the benefit of complex interventions for patients with neurocognitive disorders in our country, so this study will provide useful information for the development of care programs for this population and their families (8).
Material and Methods
This is an observational study of 25 older adults who attended the partial hospitalization service between 2017 and 2018, who received the multimodal intervention, with an attendance ratio of 65% or greater, with a Minimental State Examination greater than or equal to 10, and with caregiver availability to attend follow-up meetings.
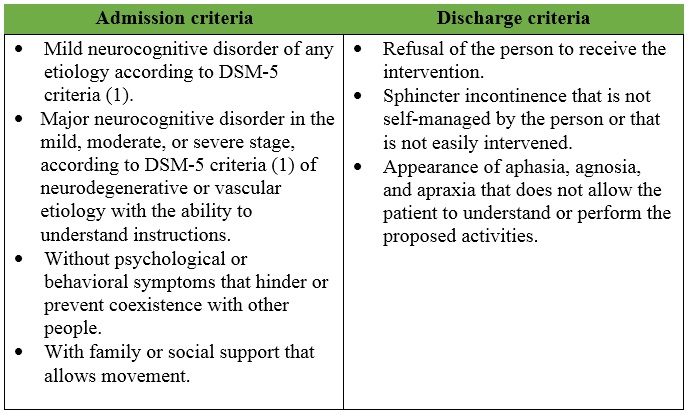
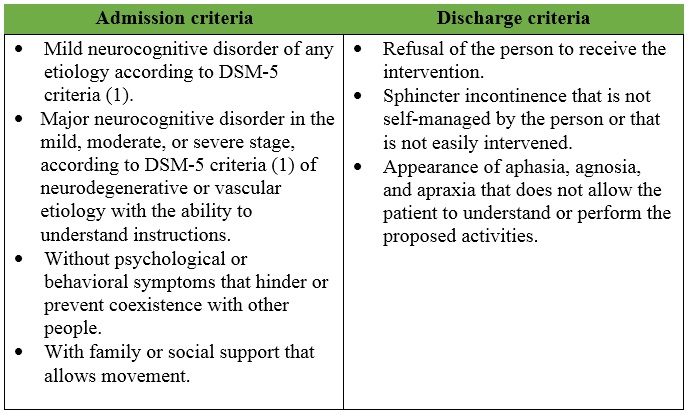
The psychogeriatric day hospital provides a multimodal intervention consisting of the stimulation of cognitive skills, periodic monitoring of the cognitive, functional, clinical, and social status of the patients, and psychoeducation of family members. The criteria for admission and discharge from the program are described in Table 1.
Table 1
Admission and discharge criteria for psychogeriatric day hospitals
Cognitive stimulation is performed by occupational therapists and is based on different models such as reality orientation, reminiscence, music therapy, and cognitive training. Different activities are used, such as sheets of paper, primers, books, and interactive software programs (functions such as attention, memory, language, executive functions, calculation, and perception are worked on alternately) (5,6).
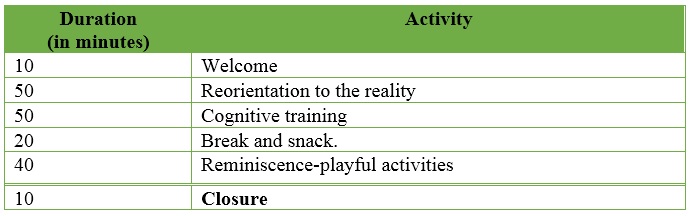
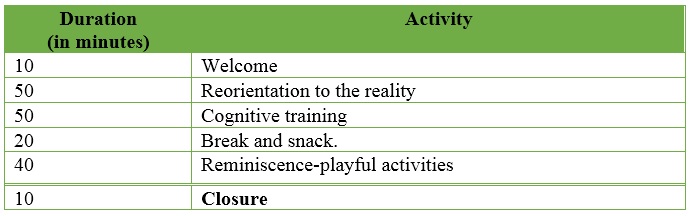
The sessions last three hours and follow the same structure (Table 2). They are developed as follows: In the first ten minutes: participants are welcomed; subsequently, reorientation activities to reality are offered, and then, different cognitive training activities are developed. Afterward, there is a twenty-minute rest period. Finally, playful activities that favor social interaction are sought.
Table 2
Cognitive stimulation session
The multimodal intervention includes periodic follow-up of the patient through the analysis of his or her evolution, which is carried out in the weekly multidisciplinary meeting. In addition, group psychoeducation meetings for families and caregivers are included once a month, designed to deal with general topics related to the pathology, its management and care, the care of the family member or caregiver, and individual or family group meetings with the psychology area, to receive specific advice on the management of grief and complex situations in the process.
In this investigation, patients were assessed at three points in time: at the beginning of the observation, at six months, and at one year. Functionality was assessed through the Barthel Scale and the Lawton Index (9); cognition, with the Montreal Cognitive Assessment (MoCA) (10); quality of life, using the Quality of Life in Alzheimer's Disease (QoL-AD) (11), and observational monitoring of stress during therapy, through the Non-Pharmacological Therapy Experience Scale (NPT-ES) (12). Informed consent was obtained from the participants' relatives, and they were also informed and expressed their agreement. All variables were analyzed using the Student's t-test. In addition, the variables Barthel, Lawton, MoCA, QoL-AD, and NPT-ES were analyzed with statistical significance tests to find the .-value.
Results
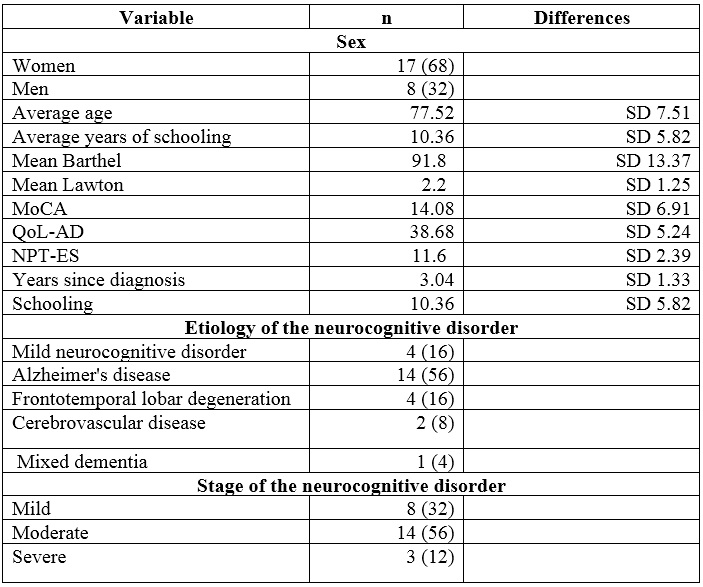
Table 3 describes the demographic characteristics of the participants. The mean age was 77.52 years (SD: 7.51). Sixty-eight percent of the participants were women, and the mean number of years of schooling was 10.36 (SD: 5.82). In 56% of the cases, the most frequent diagnosis was major neurocognitive disorder, due to Alzheimer's disease in the moderate stage. On average, patients had 3.04 years of evolution since clinical diagnosis. At six months, treatment adherence was 76.16%, with 39.6 sessions (SD: 12.43), and at one year, it was 69.29%, with 72.06 sessions (SD: 15.00).
Table 3
Baseline demographic characteristics of participants
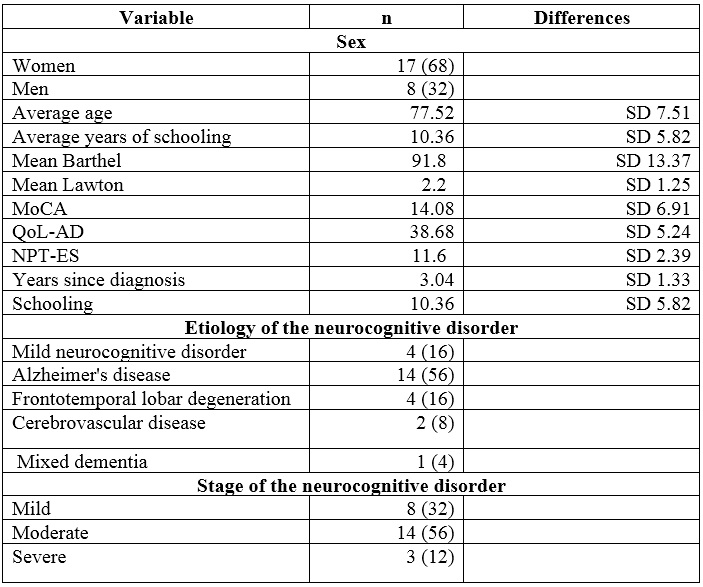
SD:standard deviation.
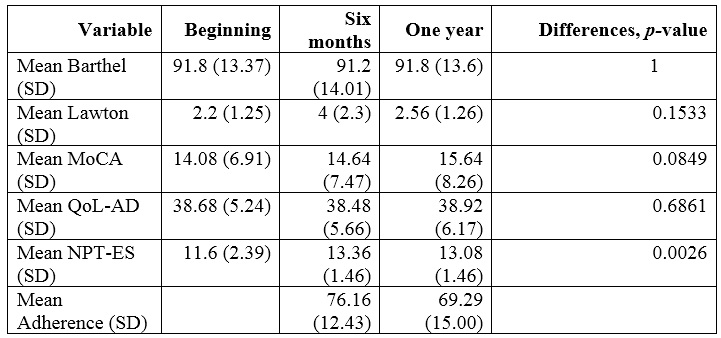
The average Barthel, Lawton, MoCA, and NPT-ES scores with their standard deviations, measured at baseline, six months, and one year are summarized in Table 4, as well as the p-value, obtained after statistical significance analysis.
Table 4
Differences in participant outcomes at six months and one year concerning baseline
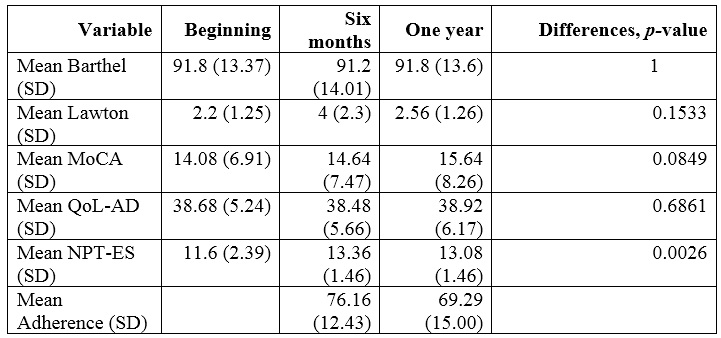
SD:standard deviation
No statistically significant differences were found in the Barthel Scale score, the Lawton Index, the MoCA test, and the QoLAD; however, in all tests, there was evidence of a trend towards improvement. This means that the participants maintained their physical, cognitive functions, and well-being during one year of treatment follow-up. A statistically significant difference was found in participants' enjoyment of therapy, as measured by the NPT-ES, meaning that the stress associated with undergoing treatment progressively decreased during the one-year follow-up.
Discussion
Currently, treatment for people living with dementia and their families presents a health care challenge. On the one hand, no drug has demonstrated a permanent benefit in delaying the progression of neurodegeneration nor are there drugs with curative effects; hence the main focus of treatment is palliative, for the control of cognitive, behavioral, and psychological symptoms, and the maintenance of the quality of life of the person and his or her family (13).
With these objectives in mind, certain findings have suggested that non-pharmacological treatments benefit cognitive domains, slow functional loss, and improve social interaction (14,15). This is why the development of studies that can expand the knowledge about the effects of nonpharmacological therapies and that, in addition, are conducted locally can favor the access of a part of society to these treatments.
Our model of care centered on the person and his or her family has as its task the permanent assessment of the evolution of the people who participate in the intervention. The Barthel Scale scores, the Lawton Index, the MoCA test, and the quality of life measured with the QOL-AD indicated that people maintained their physical functionality and cognitive status one year after starting treatment, factors that are associated with the perception of quality of life (16).
This observation has limitations. For example, we could not determine the effect of other treatments received by the patients. In addition, the patient sample was small. Therefore, we consider it relevant to carry out intervention studies with larger samples, as well as with control of confounding factors and longer observation periods. Our work is the first in the country to study the evolution of people who receive a multimodal non-pharmacological intervention.
Individuals must receive multimodal treatment given the multifactorial nature of the neurocognitive disorder and the multiplicity of symptoms that result from the pathology.
Funding
The study was conducted within the framework of the PHC-Oriented Health Interventions and Reduction of the Burden of Mental Disorders Generating Increased Chronicity and Disability program.
Conflict of Interest
None.
References
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). Washington: American Psychiatric Pub; 2013.
2. World Health Organization. Public health response to dementia [Internet]. 2021. Available from: https://www.who.int/publications/i/item/9789240033245
3. Context, framing and synergies [Internet]. 2017 [citado 2022 ene 22]. Available from: http://www.who.int/mental_health/action_plan_2013/en/
4. Sousa L, Neves MJ, Moura B, Schneider J, Fernandes L. Music-based interventions for people living with dementia, targeting behavioral and psychological symptoms: a scoping review. Int J Geriatr Psychiatry. 2021;36(11):1664-90.
5. Macleod F, Storey L, Rushe T, McLaughlin K. Towards an increased understanding of reminiscence therapy for people with dementia: a narrative analysis. Dementia. 2021;20(4):1375-407.
6. Rai H, Yates L, Orrell M. Cognitive stimulation therapy for dementia. Clin Geriatr Med. 2018;34(4):653-65.
7. Meyer C, O’Keefe F. Non-pharmacological interventions for people with dementia: a review of reviews. Dementia. 2020;19(6):1927-54.
8. Chalfont G, Milligan C, Simpson J. A mixed methods systematic review of multimodal non-pharmacological interventions to improve cognition for people with dementia. Dementia. 2020;19(4):1086-130.
9. Chavarro-Carvajal DA, Heredia Ramírez RA, Venegas Sanabria LC, Caicedo Correa SM, Gómez Arteaga RC, Pardo Amaya AM, et al. Escalas de uso frecuente en Geriatría [Internet]. Pontificia Universidad Javeriana; 2020. Available from: http://hdl.handle.net/10554/53402
10. Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005 Apr 1;53(4):695-9. https://doi.org/10.1111/j.1532-5415.2005.53221.x
11. Torres-castro S, Gutiérrez-robledo LM, Rosas-carrasco Ó, Torres-arreola LP, Guerra-silla MDG, Torres-castro S, et al. Validación de la escala Quality of Life in Alzheimer’s Disease (QOL-AD) en pacientes mexicanos con demencia ti. Neurología. 2010;51:72-80. https://doi.org/10.33588/rn.5102.2009648
12. Olazarán J, Reisberg B, Clare L, Cruz I, Peña-Casanova J, Del Ser T, et al. Nonpharmacological therapies in Alzheimer’s disease: a systematic review of efficacy. Dementia and Geriatric Cognitive Disorders. 2010;30(2):161-78. https://doi.org/10.1159/000316119
13. Shaji KS, Sivakumar PT, Rao GP, Paul N. Clinical Practice Guidelines for Management of Dementia. Indian J Psychiatry. 2018 Feb;60(Suppl 3):S312-S328. https://doi.org/10.4103/0019-5545.224472
14. Saragih ID, Tonapa SI, Saragih IS, Lee BO. Effects of cognitive stimulation therapy for people with dementia: a systematic review and meta-analysis of randomized controlled studies Int J Nurs Stud. 2022 Apr;128:104181. https://doi.org/10.1016/j.ijnurstu.2022.104181
15. Ham MJ, Kim S, Jo YJ, Park C, Nam Y, Yoo DH, et al. The effect of a multimodal occupational therapy program with cognition-oriented approach on cognitive function and activities of daily living in patients with Alzheimer’s disease: a systematic review and meta-analysis of randomized controlled trials. Biomedicines. 2021;9(12). https://doi.org/10.3390/biomedicines9121951
16. Stewart-Archer LA, Afghani A, Toye CM, Gomez FA. Subjective quality of life of those 65 years and older experiencing dementia. Dementia. 2016;15(6):1716-36. https://doi.org/10.1177/1471301215576227
Author notes
a Correspondence author: goviedo@javeriana.edu.co
Additional information
How to cite: Gama González AC, Oviedo Lugo GF, Vargas Fonseca S, Benito Cuadrado M, Giraldo Villate CI. Does a multimodal intervention have any effect on people with a neurocognitive disorder? Univ. Med. 2022;63(2). https://doi.org/10.11144/Javeriana.umed63-2.imul