Introduction
With the emergence of SARS-CoV-2, the world's healthcare services were forced to take drastic health measures to mitigate the impact of COVID-19. At the beginning of the pandemic, due to high hospital occupancy, the need to reserve intensive care unit (ICU) beds for COVID-19 infected patients, as well as in an attempt to reduce infection rates and postoperative morbidity and mortality, surgical services were forced to avoid elective surgeries and to admit only emergency patients under strict biosafety protocols (1).
Before the COVID-19 pandemic, according to data from the International Study Group on Surgical Outcomes in Elective Surgery Patients, 16.4% of patients required ICU after surgery, and 16.8% had some complication, including: arrhythmias (2.7%), acute myocardial infarction (0.3%) and pulmonary embolism (0.2%). The described 30-day postoperative mortality was 0.5% (2). Other studies such as GlobalSurg 2 found 30-day mortality following gastrointestinal procedures of 1.9%, which varies according to the income level of the countries, with 30-day mortality being 1.5 % in high-income countries and 4.8% in low-income countries (3).
During the COVID-19 pandemic, an increase in postoperative complications and mortality was evident, especially in the period prior to the start of the SARS-CoV-2 vaccination. According to CovidSurg data, 30-day mortality in patients undergoing surgery with perioperative SARS-CoV-2 infection reached 23.8%. Half of these patients (51.2%) had pulmonary complications, predominantly pneumonia (42.1%), and an increased length of hospital stay of more than 30 days was also observed in 22.9% of patients (4). These findings may be related to the altered immune response resulting from SARS-CoV-2 infection, coupled with the excessive immune response typical of the postoperative state, especially in patients with major cardiothoracic and gastrointestinal surgery and oncology patients, which is characterized by increased serum concentrations of cytokines such as IL-6, IL-8, and TNF-alpha (5,6).
Colombia had a high cumulative incidence of COVID-19, which between September and November 2020 reached 81,217 cases per million population (7). Also, there was a variable seroprevalence of antibodies against SARS-CoV-2 between October and November 2020, ranging from 27% to 33% in Bogotá (8,9). During the first epidemic wave, around October 2020, and as elective procedures could no longer be postponed, national guidelines were issued on the prioritization of procedures, based on a local SARS-CoV-2 RT-PCR positivity rate of less than 20% (10). To this end, it was recommended to implement symptom screening surveys, measurement of predictive scales for prioritization such as MentS (11), preoperative virus testing, and special routes for patient transfer (12).
The objective of this study was to describe the cumulative postoperative COVID-19 incidence and 30-day mortality following urgent or elective surgical procedures during most of the first three epidemic waves in Colombia between March 6, 2020, and June 30, 2021, at the Hospital Universitario San Ignacio (HUSI).
Materials and methods
A descriptive-retrospective study was designed, for which a random sample of patients who were taken for urgent or elective surgical procedures from March 6, 2020 to June 30, 2021, at HUSI, was collected. Patients aged 18 years or older were included. Interventional radiology procedures and those performed in hemodynamic wards were excluded. All patients undergoing elective surgery had nasopharyngeal swabs taken to process RT-PCR for SARS-CoV-2 preoperatively.
314 patients were randomly selected from the target population (n = 11,345), taking into consideration a hypothetical prevalence of 30% of SARS-CoV-2 in the population, based on prevalence data in Bogotá for October 2020 with a 95% confidence interval (9).
Data were reviewed and extracted from the electronic medical records, whose records correspond to the standard care of these patients in the HUSI. These data were stored in the web application Research Electronic Data Capture (REDCap), in a form that had filters and restrictions for data entry. All data were anonymized using a unique code per patient. To ensure the reliability and veracity of the information, the medical coordinator of the study reviewed 10% of the data entered weekly until data collection was completed. Demographic variables, patient history, and preoperative assessment were recorded, ASA classification, postoperative follow-up, need for ICU admission, respiratory and hemodynamic complications, and requirement for invasive mechanical ventilation, as well as in-hospital mortality associated with or attributed to COVID-19 and all-cause mortality.
Patients were followed up to 30 days after the surgical procedure, either by review of medical records if they remained hospitalized, or by review of telephone records between days 7 and 30 postoperatively. Perioperative COVID-19 cases were recorded, defined as patients who had a positive PCR for SARS-CoV-2 30 days before or 30 days after the surgical procedure. Additionally, in patients with perioperative COVID-19, mortality was calculated, differentiating mortality between patients with and without preoperative COVID-19.
As secondary objectives, we assessed perioperative morbidity and complications, specifically the frequency of the need for ICU, mechanical ventilation, occurrence of acute respiratory distress syndrome (ARDS), acute kidney injury, and myocardial injury, prior to and within 30 days after the surgical procedure in the study population. Postoperatively, the occurrence of operative site infection (OSI), seroma, bleeding, hematoma, anastomotic dehiscence, evisceration, and unplanned reoperation at 30 days were described.
This project was presented and endorsed by the Institutional Research and Ethics Committee of the Pontificia Universidad Javeriana and HUSI with code 2022/225. As this was a minimal risk research, informed consent was not requested.
Statistical analysis
All analyses were carried out with R software (version 4.1). Nominal variables were described as percentages, while ordinal variables were described as proportions and quartiles. Meanwhile, continuous variables were described as means and standard deviations, or medians and interquartile ranges (IQR), according to the distribution of the data.
To assess the cumulative incidence of postoperative COVID-19, the numerator was new infections confirmed by RT-PCR for SARS-CoV-2 postoperatively, and the denominator was the study population, excluding patients with SARS-CoV-2 infection within 90 days prior to the surgical intervention. Within the follow-up of this cohort of patients, no postoperative molecular testing was performed; only those who presented with COVID-19-related symptoms.
Results
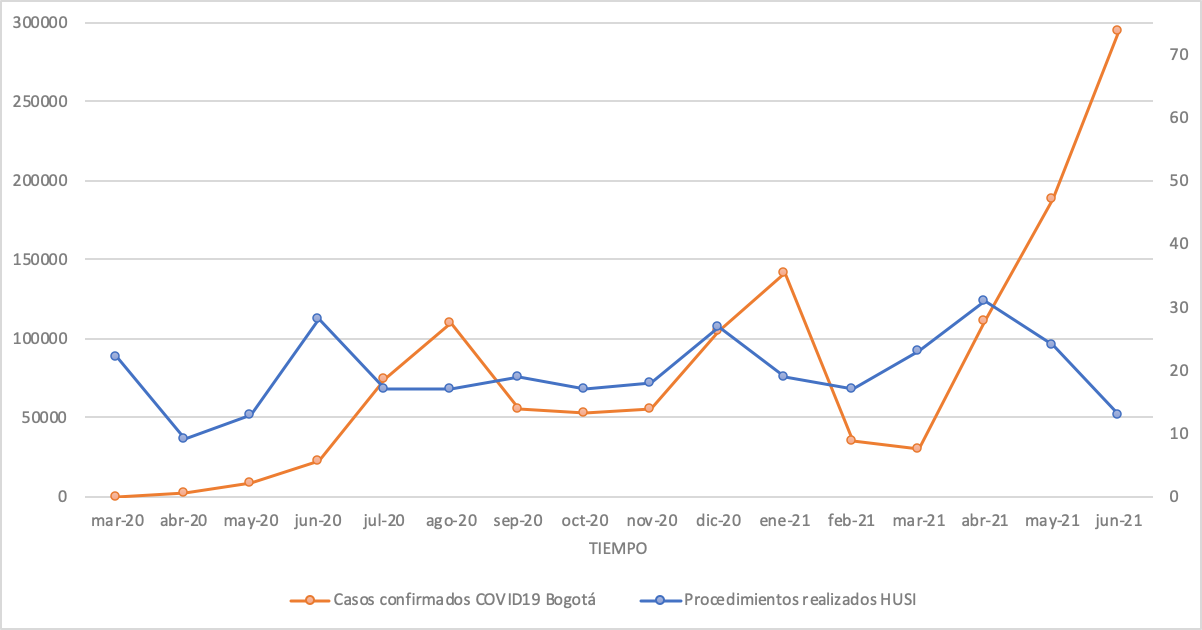
Of the 314 patients with surgical interventions, 51% (n = 160) were male, and the majority were between 40 and 69 years of age (54.1%; n = 170). The distribution of surgical interventions over time is presented in Figure
1.
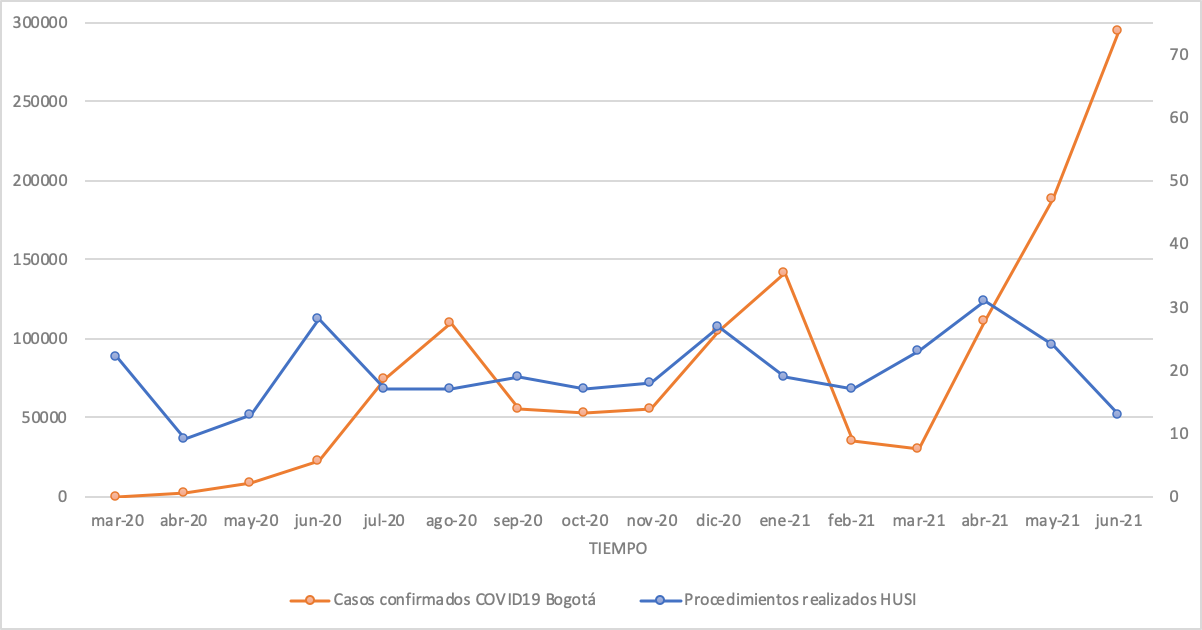 Figure 1.
Distribution of confirmed COVID-19 cases in Bogotá versus distribution of surgical procedures in the study population at the Hospital Universitario San Ignacio, March 2020-June 2021
Figure 1.
Distribution of confirmed COVID-19 cases in Bogotá versus distribution of surgical procedures in the study population at the Hospital Universitario San Ignacio, March 2020-June 2021
Note. The distribution of COVID-19 cases in the city of Bogotá is shown (in orange), according to data registered in SaludData (https://saludata.saludcapital.gov.co/osb/index.php/datos-de-salud/enfermedades-trasmisibles/covid19/). Note that three epidemic peaks occurred during the study period: the first between June and September 2020, the second between December 2020 and January 2021, and the third starting in April 2021 and continuing until June 2021. The distribution of surgical procedures at HUSI is shown in blue. The comparison shows that during epidemic peaks the number of surgical procedures decreased.
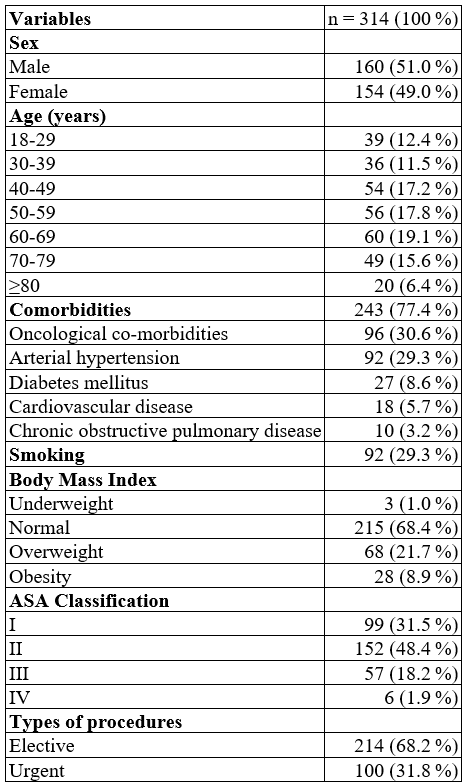
A total of 243 comorbidities were documented. Sixty-eight percent (n = 214) of the patients had at least one comorbidity, taking into account that some patients could have more than one comorbidity at the same time. The two most frequent were hypertension and oncological diseases, and both together affected 59.9% (n = 188) of the cases. Among the patients whose Body Mass Index was calculated, 30% (n = 96) were overweight or obese (Table 1).
Table 1.
Clinical description of a surgical patient population
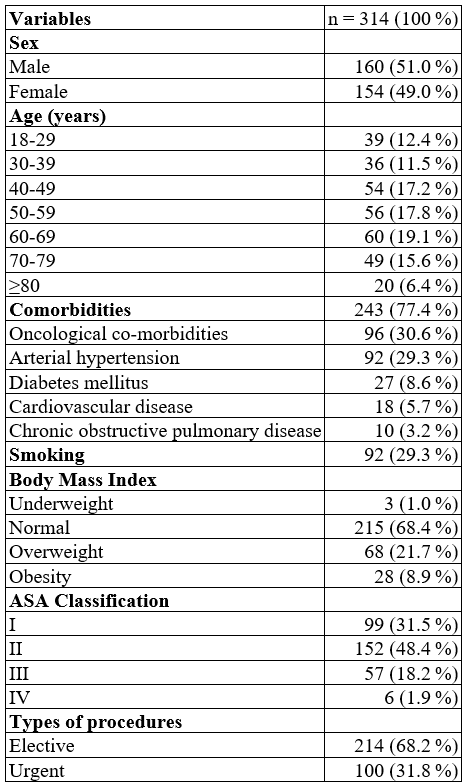
Acute appendicitis was the most frequent preoperative diagnosis in 4.8% (n = 15) of cases. The majority of surgical procedures were elective (68.2%; n = 214). The most frequent surgical approach was open (58.0%; n= 182) and the median operative time was 80 minutes (IQR: 50-120). Most patients were classified as ASA II (see Table 1).
The specialty with the highest frequency of surgical procedures was general surgery, 29.3% (n = 92), followed by orthopedics, 17.1% (n = 54), and urology, 6.7% (n = 21). The most frequently repeated surgical procedures were cholecystectomy (6.7%; n = 21), fracture reduction and fixation (5.1%; n = 16) and appendectomy (3.5%; n = 11). 2.2 % (n = 7) of patients developed complications during the procedure, but no patient died intraoperatively (see Table 1).
The most frequent complication was surgical site infection (SSI) in 3.2% (n = 10) of patients, of which superficial SSI was the most common (2.9%; n = 9), and there was only one case of organ-space type SSI (0.3%; n = 1). The overall 30-day mortality was 2.2% (n = 7). Of these deaths, 4 cases were not associated with COVID-19, and the rest were associated with COVID-19.
SARS-CoV-2 infection
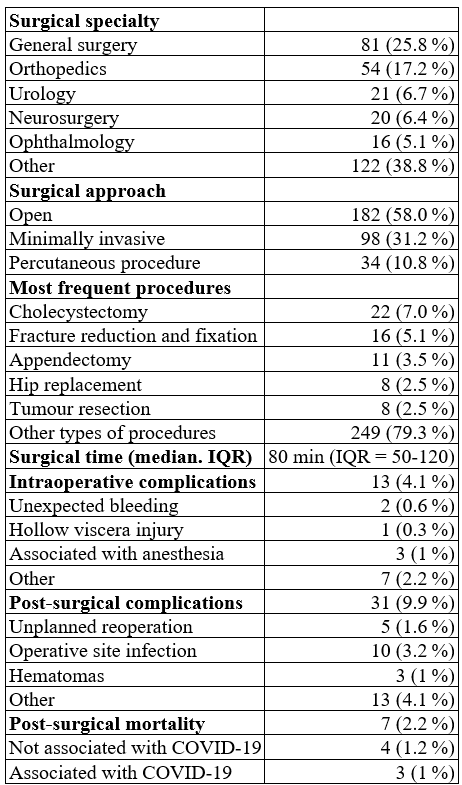
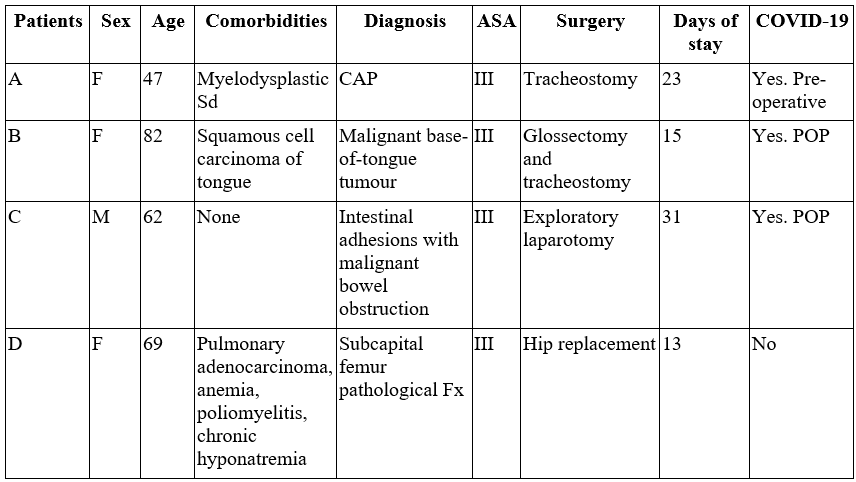
In the perioperative period, 7 patients had SARS-CoV-2 infection, while 4 had preoperative infection and required urgent or essential elective surgery (13). Tracheostomy for prolonged orotracheal intubation was indicated in 3 of the cases, as these patients had ARDS. The median time between diagnosis and tracheostomy was 21 days (ICR: 19-25). The fourth patient had acute occlusive arterial disease with critical ischemia, with an indication for lower limb amputation; however, on admission, he had respiratory symptoms confirmed for severe COVID-19, so surgery was deferred until 17 days later after reaching clinical stability. One of the patients with an indication of tracheostomy died within 30 days postoperatively. This patient had myelodysplastic syndrome with severe secondary pancytopenia and organizing pneumonia secondary to SARS-CoV-2 as the main diagnoses, and his death was considered to be associated with COVID-19 (Table 2).
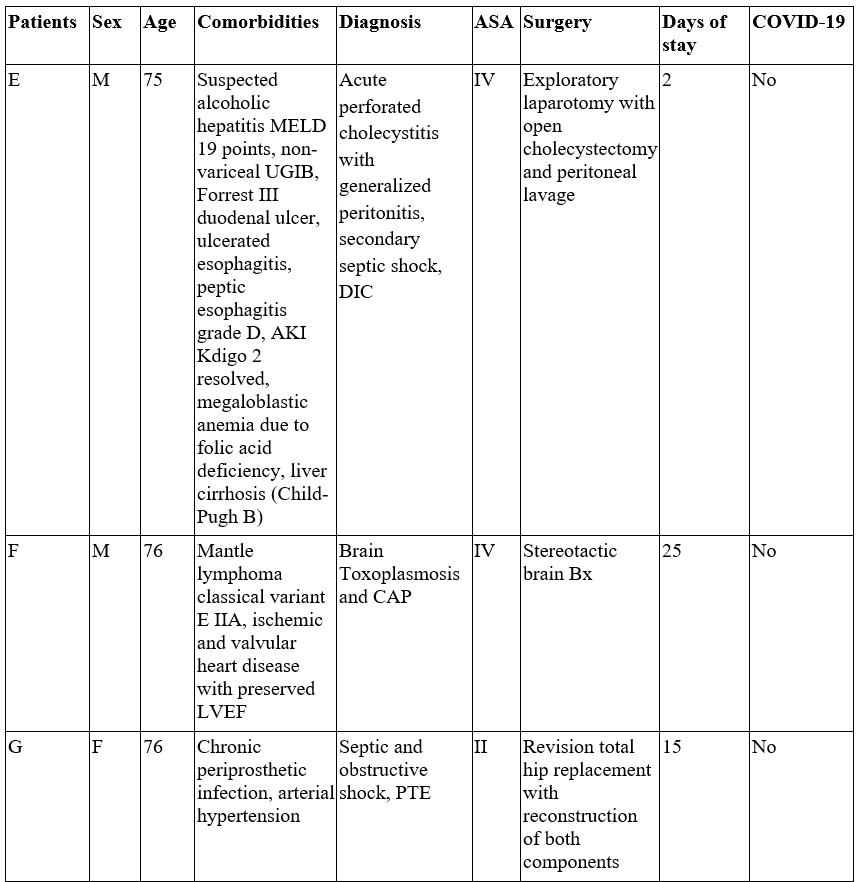
Table 2.
Perioperative mortality in the surgical patient population
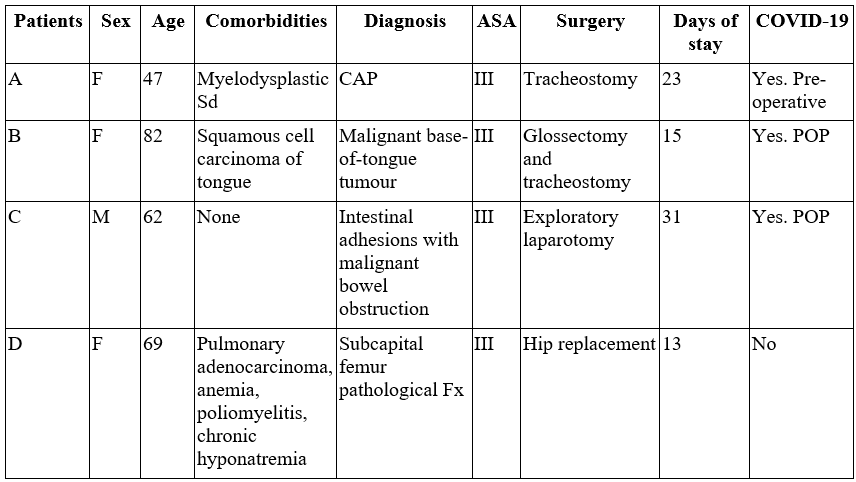
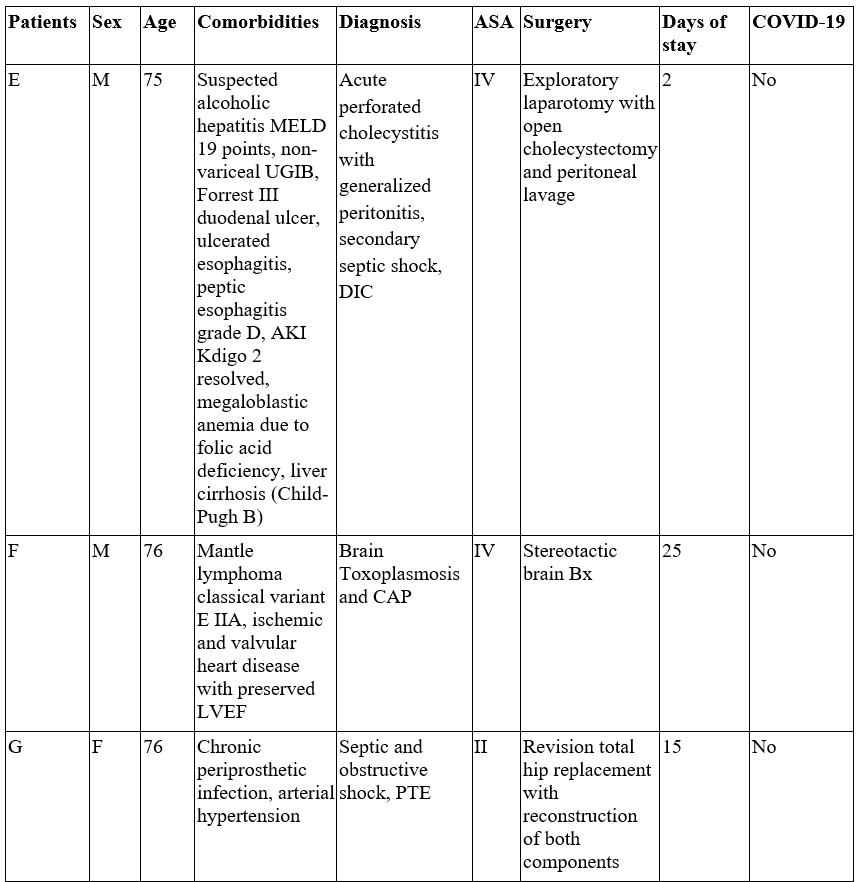
AKI: acute kidney injury; Bx: biopsy; CAP: community-acquired pneumonia; DIC: disseminated intravascular coagulation; Fx: fracture; LVEF: left ventricular ejection fraction; MELD: Model for End-stage Liver Disease; POP: post-operative; PTE: pulmonary thromboembolism. Sd: Syndrome; UGIB: upper gastrointestinal tract bleeding.
Three cases of incident COVID-19 were detected postoperatively, with a median between procedure and positive test of 9 days (Interquartile range (IQR): 7-15). This calculated a cumulative incidence of 0.97% at 30 days. Two of these patients died. The first one had a squamous cell carcinoma of the tongue and required elective-urgent surgery for a radical glossectomy with gastrostomy and tracheostomy, with a negative preoperative molecular test for SARS-CoV-2; however, 7 days postoperatively, COVID-19 infection was confirmed. This patient had a torpid evolution with complications such as pulmonary thromboembolism (PTE), secondary bacterial infection, and refractory response to medical management, for which palliative management was performed until her death. The second patient who died had an intestinal obstruction due to a malignant tumor, and was taken to emergency surgery for mass resection and lysis of adhesions; but 15 days later, COVID-19 was confirmed by molecular testing, with a torpid evolution, and indication for orotracheal intubation, which he refused. The patient died 21 days after the procedure with associated mortality (see Table 2).
Discussion
In our study, we found a cumulative incidence of COVID-19 30 days after the surgical procedure of 0.97% (95% CI: 0.95-0.99) in both elective and emergency surgeries in a tertiary-level university hospital in the city of Bogotá (Colombia). When comparing this incidence with other descriptive studies from Spain, the United States, and Iraq, there is a range of documented incidence from 0.5% to 7% (13,14,15), so we observed a similar incidence of infection in our cohort. The high incidences reported in some studies are related to the selection of high-risk populations, such as oncology patients, and major surgeries, or because they were reported at the beginning of the pandemic when less restrictive behaviors were taken for surgical interventions (13,14,15).
In the cohort of patients who underwent surgery, 9.9% had some complications, most of them infectious; 3.3% had SSI, and 90% of these were superficial. Based on this finding, there appears to be no increase in the incidence of SSI compared to what was reported before the pandemic. The GlobalSurg study reported a rate of 5.0% in 27 countries of different incomes in 2014 in elective surgeries (2), and is consistent with evidence from other studies done during the pandemic (16,17,18). This finding may be related to the high adherence to biosecurity measures for the prevention of SARS-CoV-2 infection, which are also effective for the prevention of SSI (16,17,18).
Postoperative complications in patients with perioperative COVID-19 were frequent in our study. We reported a requirement for invasive mechanical ventilation in 57.1% (4 out of 7) and the occurrence of ARDS in 28.6% (2 out of 7), which is consistent with that reported by other authors (4,19). These findings reinforce the need to restrict elective procedures and to follow strict protocols in operating rooms, such as preoperative RT-PCR for SARS-CoV-2 in elective surgeries, at times of pandemic peaks, with a high incidence of SARS-CoV-2 in the community and low vaccination coverage, following national and international evidence-based recommendations generated during the pandemic (10,12,20).
The 30-day perioperative mortality in patients undergoing surgery in our population was 2.2% (95% CI 2.0-2.4). According to international multicentre registries prior to 2020, the expected mortality was 0.5-4.8% (2.3), and in studies published during the pandemic, mortality ranged from around 2.0% to 7.9% (21, 22). Therefore, there does not appear to be an overall excess of mortality in our population compared to the pre-pandemic period, nor during it. The scenario is different in patients with perioperative COVID-19, where we report mortality in 3 of 7 patients (42,8%).
Published data show a high mortality rate of between 12.8 % and 66.0% (4,19,21,22,23,24,25,26) in patients with this disease. Mortality in all the patients we reported was associated and may be explained by their comorbidities; additionally, in all cases, the surgical interventions were urgent or elective-priority and could not be postponed, so they were not preventable events. These findings reinforce the need to avoid closing operating rooms during pandemics and the importance of conducting risk-based protocols and priority of procedures to maintain a risk-benefit balance for patients before surgical procedures during pandemics (16).
There are several weaknesses in our study. It is a descriptive cohort study that is designed exclusively to calculate frequency measures and not to report measures of association between COVID-19 and the observed outcomes. In addition, it is a single-center study, conducted in a fourth-level, accredited university hospital, so the results cannot be extrapolated to the general Colombian population. In addition, no vaccination data are included in the cohort analyzed, since by the end of the follow-up period, the national vaccination plan for the prioritized population was only just being initiated, so their results show the pre-vaccination situation.
The evidence published to date amply demonstrates the benefit of vaccination before surgical interventions. In patients with a complete vaccination schedule, a decrease in pulmonary (OR: 0.54 [0.39-0.72]) or thrombotic complications (OR: 0.68 [0.46-0.99]), and hospital length of stay (OR: 0.78 [0.69-0.89]) was observed (27). Partial vaccination, at least one dose, and even prior exposure to COVID-19 also showed benefits, especially in the prevention of pulmonary complications (27,28). There is already sufficient evidence that vaccination at least 14 days before a surgical procedure is useful in preventing COVID-19 infection, as well as the occurrence of complications (29).
As the two most relevant findings of our results, we highlight the low incidence of postoperative COVID-19 and the low overall mortality in the surgical population. These provide information and evidence about the safety of patients undergoing surgery during a pandemic following strict, evidence-based care protocols (10). With the increase in time for non-urgent surgery due to the pandemic, there were undesirable outcomes. The main effects observed in a global study of cancer patients scheduled for surgical treatment were: at least 1 in 7 patients did not undergo scheduled treatment for pandemic-related reasons; times of severe restrictions were associated with a delay of more than 6 weeks for surgery; 22.6% of patients had to be re-staged due to waiting time; and 8.9% of patients progressed to unresectable pathology (30,31).
The experience with the SARS-CoV-2 pandemic and the measures adopted serve as a precedent for future health crises secondary to infectious diseases involving increased morbidity and mortality secondary to surgical procedures, in which scenario it is essential to maintain a balance between restrictive and inclusive behaviors to mitigate risks to patients and lead to the best health outcomes in periods of healthcare emergencies.
Funding
This work was funded by the HUSI. We declare that we have not received individual or group funding from any other public or private entity.
Conflict of interests
The authors of this article declare that we have no conflict of interest.
Acknowledgments
To the Pontificia Universidad Javeriana and HUSI, for allowing us to develop studies that contribute to the construction of knowledge, innovation and technology for the nation.
References
1. COVIDSurg Collaborative; GlobalSurg Collaborative. Timing of surgery following SARS-CoV-2 infection: an international prospective cohort study. Anaesthesia. 2021 Jun;76(6):748-58. https://doi.org/10.1111/anae.15458
2. International Surgical Outcomes Study Group. Global patient outcomes after elective surgery: prospective cohort study in 27 low-, middle- and high-income countries. Br J Anaesth. 2016 Oct 31;117(5):601-9. https://doi.org/10.1093/bja/aew316
3. GlobalSurg Collaborative. Surgical site infection after gastrointestinal surgery in high-income, middle-income, and low-income countries: a prospective, international, multicentre cohort study. Lancet Infect Dis. 2018 May;18(5):516-25. https://doi.org/10.1016/S1473-3099(18)30101-4
4. COVIDSurg Collaborative. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020 Jul 4;396(10243):27-38. https://doi.org/10.1016/S0140-6736(20)31182-X
5. Kaufmann KB, Heinrich S, Staehle HF, Bogatyreva L, Buerkle H, Goebel U. Perioperative cytokine profile during lung surgery predicts patients at risk for postoperative complications-A prospective, clinical study. PLoS One. 2018 Jul 3;13(7):e0199807. https://doi.org/10.1371/journal.pone.0199807
6. Besnier E, Tuech JJ, Schwarz L. We asked the experts: COVID-19 outbreak: is there still a place for scheduled surgery? Reflection from pathophysiological data. World J Surg. 2020;44:1695-8. https://doi.org/10.1007/s00268-020-05501-6
7. Instituto Nacional de Salud. Coronavirus (COVID-19) en Colombia [Internet]. 2020-2023 [cited 2023 Jan 10]. Available from: https://www.ins.gov.co/Noticias/Paginas/Coronaviruss.aspx
8. Instituto Nacional de Salud. Estudio nacional de seroprevalencia de SARS-CoV-2 [Internet]. [Cited 2022 Dec 12]. Available from: https://www.ins.gov.co/estudio-nacional-de-seroprevalencia/reporte.html
9. Mercado M, Malagón J, Rodríguez I, Zapata S, Wiesner M, Cucunubá Z, et al. Seroprevalence of anti-SARS-CoV-2 antibodies in Colombia, 2020: a population-based study. Lancet Reg Health Am. 2022 May;9:100195.
10. Saavedra Trujillo CH, et al. Consenso colombiano de atención, diagnóstico y manejo de la infección por SARS-COV-2/COVID-19 en establecimientos de atención de la salud. Infectio. 2020;24(3 supl 1):88-100. https://doi.org/10.22354/in.v24i3.851
11. Prachand VN, Milner R, Angelos P, Posner MC, Fung JJ, Agrawal N, et al. Medically necessary, time-sensitive procedures: scoring system to ethically and efficiently manage resource scarcity and provider risk during the COVID-19 pandemic. J Am Coll Surg. 2020 Aug;231(2):281-288. https://doi.org/10.1016/j.jamcollsurg.2020.04.011
12. Torregrosa L, Prieto RG, Cabrera LF, Ordóñez J, Sánchez E, Rodríguez C, et al. Recomendaciones generales para los servicios de cirugía en Colombia durante la pandemia COVID-19 (SARS-CoV-2). Rev Colomb Cirug. 2020;35(2):265-81. https://doi.org/10.30944/20117582.633
13. Di Martino M, García J, Maqueda R, Muñoz JL, de la Hoz A, Correo A, Martín E. Cirugía electiva durante la pandemia por SARS-CoV-2 (COVID-19): análisis de morbimortalidad y recomendaciones sobre priorización de los pacientes y medidas de seguridad. Cir Esp. 2020;98(9):525-32. https://doi.org/10.1016/j.ciresp.2020.04.029
14. Prasad NK, Lake R, Englum BR, Turner DJ, Siddiqui T, Mayorga-Carlin M, et al. Increased complications in patients who test COVID-19 positive after elective surgery and implications for pre and postoperative screening. Am J Surg. 2022 Feb;223(2):380-7. https://doi.org/10.1016/j.amjsurg.2021.04.005
15. Mohammadzadeh N, Abkhoo A, Ashouri M, Jalaeefar A, Kazemzadeh Houjaghan A, Ghorbani B, et al. Postoperative nosocomial COVID-19 infection in surgical patients during pandemic: a prospective observational cohort study. Ann Med Surg (Lond). 2022 Nov;83:104730. https://doi.org/10.1016/j.amsu.2022.104730
16. Asociación Colombiana de Infectología, Saavedra CH, et al. Prevención y control de la infección por SARS-CoV-2/COVID-19. Seccion X. Infectio. 2021;25(4):350. https://doi.org/10.22354/in.v25i4.980
17. Smith BB, Bosch W, O'Horo JC, Girardo ME, Bolton PB, Murray AW, et al. Surgical site infections during the COVID-19 era: a retrospective, multicenter analysis. Am J Infect Control. 2022 Sep 23:S0196-6553(22)00706-4.
18. Losurdo P, Paiano L, Samardzic N, Germani P, Bernardi L, Borelli M, et al. Impact of lockdown for SARS-CoV-2 (COVID-19) on surgical site infection rates: a monocentric observational cohort study. Updates Surg. 2020 Dec;72(4):1263-71. https://doi.org/10.1007/s13304-020-00884-6
19. Knisely A, Zhou ZN, Wu J, Huang Y, Holcomb K, Melamed A, et al. Perioperative morbidity and mortality of patients with COVID-19 who undergo urgent and emergent surgical procedures. Ann Surg. 2021 Jan 1;273(1):34-40. https://doi.org/10.1097/SLA.0000000000004420
20. American College of Surgeons. Local resumption of elective surgery guidance [Internet]. ACS. 2020 [cited 2023 Feb 17]. Available from: https://www.facs.org/for-medical-professionals/COVID-19/clinical-guidance/resuming-elective-surgery/
21. Inzunza M, Romero C, Irarrázaval MJ, Ruiz-Esquide M, Achurra P, Quezada N, et al. Morbidity and mortality in patients with perioperative COVID-19 infection: prospective cohort in general, gastroesophagic, hepatobiliary, and colorectal surgery. World J Surg. 2021 Jun;45(6):1652-62. https://doi.org/10.1007/s00268-021-06068-6
22. Jonker PKC, van der Plas WY, Steinkamp PJ, Poelstra R, Emous M, van der Meij W, et al.; Dutch Surgical COVID-19 Research Collaborative. Perioperative SARS-CoV-2 infections increase mortality, pulmonary complications, and thromboembolic events: a Dutch, multicenter, matched-cohort clinical study. Surgery. 2021 Feb;169(2):264-74. https://doi.org/10.1016/j.surg.2020.09.022
23. Aminian A, Safari S, Razeghian-Jahromi A, Ghorbani M, Delaney CP. COVID-19 outbreak and surgical practice: unexpected fatality in perioperative period. Ann Surg. 2020 Jul;272(1):e27-e29. https://doi.org/10.1097/SLA.0000000000003925
24. Lei S, Jiang F, Su W, Chen C, Chen J, Mei W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020 Apr 5;21:100331. https://doi.org/10.1016/j.eclinm.2020.100331
25. Doglietto F, Vezzoli M, Gheza F, Lussardi GL, Domenicucci M, Vecchiarelli L, et al. Factors associated with surgical mortality and complications among patients with and without coronavirus disease 2019 (COVID-19) in Italy. JAMA Surg. 2020 Aug 1;155(8):691-702. https://doi.org/10.1001/jamasurg.2020.2713
26. Nahshon C, Bitterman A, Haddad R, Hazzan D, Lavie O. Hazardous postoperative outcomes of unexpected COVID-19 infected patients: a call for global consideration of sampling all asymptomatic patients before surgical treatment. World J Surg. 2020 Aug;44(8):2477-81. https://doi.org/10.1007/s00268-020-05575-2
27. Prasad NK, Lake R, Englum BR, Turner DJ, Siddiqui T, Mayorga-Carlin M, et al. COVID-19 vaccination associated with reduced postoperative SARS-CoV-2 infection and morbidity. Ann Surg. 2022 Jan 1;275(1):31-6. https://doi.org/10.1097/SLA.0000000000005176
28. Prasad NK, Englum BR, Mayorga-Carlin M, Turner DJ, Sahoo S, Sorkin JD, Lal BK. Partial COVID-19 vaccination associated with reduction in postoperative mortality and SARS-CoV-2 infection. Am J Surg. 2022 Oct;224(4):1097-102. https://doi.org/10.1016/j.amjsurg.2022.03.038
29. Le ST, Kipnis P, Cohn B, Liu VX. COVID-19 vaccination and the timing of surgery following COVID-19 infection. Ann Surg. 2022 Nov 1;276(5):e265-e272. https://doi.org/10.1097/SLA.0000000000005597
30. Ciarleglio FA, Rigoni M, Mereu L, Tommaso C, Carrara A, Malossini G, et al. The negative effects of COVID-19 and national lockdown on emergency surgery morbidity due to delayed access. World J Emerg Surg. 2021 Jul 13;16(1):37. https://doi.org/10.1186/s13017-021-00382-z
31. COVIDSurg Collaborative. Effect of COVID-19 pandemic lockdowns on planned cancer surgery for 15 tumour types in 61 countries: an international, prospective, cohort study. Lancet Oncol. 2021 Nov;22(11):1507-17. https://doi.org/10.1016/S1470-2045(21)00493-9
Additional information
How to cite: Valderrama Beltrán SL, Grueso-Angulo R, Montealegre-Díaz JS, Bernal-Gutiérrez M, Cataño JG, Galvis-Navarrete SH, Ramírez-Schneider E, Torres-Ortiz MP, Portilla-Rojas E. Perioperative morbidity and mortality in patients undergoing elective and emergency surgery during COVID-19 pandemic in a fourth level hospital. Univ. Med. 2023;64(4). https://doi.org/10.11144/Javeriana.umed64-4.mmpc