INTRODUCTION
In Colombia, the liberal practice of dentistry began a gradual process of transformation when Law 100 of 1993 was enacted. The Law in its second book created the General System of Social Security in Health (SGSSS) (1), which mainly develops the contents of articles 48 and 49 of the Colombian Political Constitution (2).
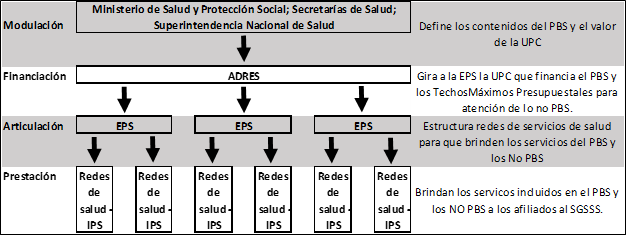
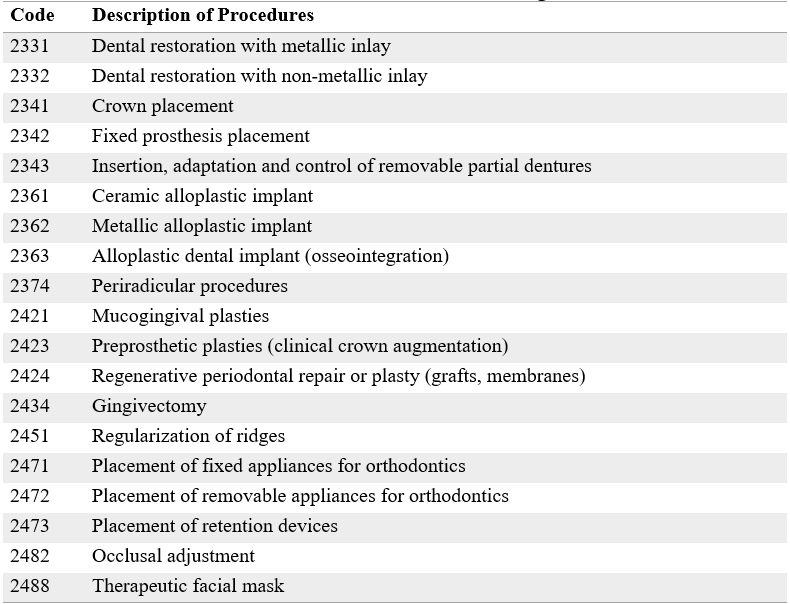
The SGSSS is based on the principles of structural pluralism, which organizes health care systems through four major functions: modulation, financing, articulation, and delivery (3). In the Colombian case, the Ministry of Health, the Superintendency of Health, and the regional health secretaries comply with the modulation. The SGSSS Resources Administrator (ADRES) is responsible for financing. Health Promoting Entities (EPSs) are in charge of the articulation. Health Services Providers (IPSs), such as hospitals, clinics, and professional practices, deliver services (1) (Figure 1).
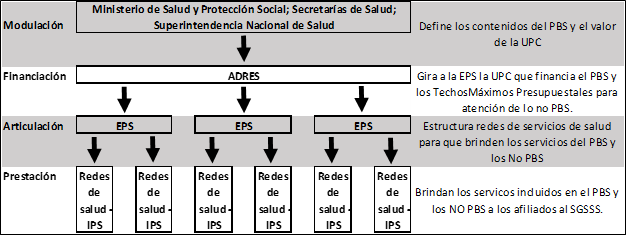 FIGURE 1
Structure of the SGSSS according to the logic of Structural Pluralism (figure in Spanish)
FIGURE 1
Structure of the SGSSS according to the logic of Structural Pluralism (figure in Spanish)
Source: the authors
In practice, structural pluralism in the SGSSS is based on an insurance model that seeks to guarantee universal coverage to all the inhabitants of the territory through their affiliation to two regimes: contributory and subsidized (1). The former includes workers with a formal employment, retirees, and independent workers with the ability to pay, together with their families (4). The latter covers poor and vulnerable populations, targeted through an instrument that identifies unmet basic needs and is called the Beneficiary Selection System for Social Programs (SISBEN) or through census lists in the case of special protection populations (5-6).
The SGSSS is managed by the EPSs that are in charge of affiliating the population, collecting, and compensating the contributions before the ADRES. Likewise, the EPSs organize the health care networks, through the contracting of IPSs, with which they must guarantee to all affiliates the provision of the services contained in the package of procedures, activities, interventions, supplies, and medications, which initially it was called the Obligatory Health Plan (POS) (1) and was later renamed the Health Benefits Plan (PBS) (4,6-7).
Since the beginning of the SGSSS, a significant number of services and technologies for oral health care have been incorporated into the PBS, which the country's inhabitants have been able to access without having to pay out-of-pocket costs. In this system, citizens, companies, and the government finance the costs through payroll parafiscal contributions and national and territorial taxes (1,4). In Colombia, health care became, after a long process of social struggles and constitutional and legal advances, a Fundamental Right protected by the State for all its citizens (8-9).
In practice this meant, to a large extent, a reduction of dentistry as a private practice. In that type of practice, the dentist-patient relationship is not mediated by any public or private agent and leaves it in the hands of supply-and-demand laws that are typical of free markets (10-13). They also determine treatment prices. Such laws provide clinical care guidance and codes of ethics and deontology (14). The reduction in private practice was offset by the expansion of institutionalized practice that, under the previous National Health System, had already been taking place in the Social Security Institute, social security funds, family compensation funds, health departments, and public hospitals (15-16). In the SGSSS, it began to be conducted through public, private, or public-private EPSs and IPSs.
Institutionalized practice is characterized by the fact that the conditions of clinical practice must respond and adjust to what is regulated within the normative corpus, in this case, the SGSSS and those of each institution. The latter are sometimes used to generate access barriers of various kinds (i.e., geographic, economic, administrative, cultural, and technological) that hinder and prevent health care for members, especially the poorest and most vulnerable, becoming this a contradiction of the philosophical orientation of the SGSSS and the fundamental right to health (17-19).
In addition, the institutionalization of dental practice was not accompanied by a growth in jobs that provided decent contracts and working conditions for all dentists, to a large extent, because the actual coverage of oral health services compared to those required by the population has been low (20,21). As a result, this type of contracts became restricted, almost exclusively, to the limited offers from EPSs and IPSs that provide the PBS. This situation was aggravated by the measures taken to control the Covid-19 pandemic, which raised the unemployment rate and reduced the economic income of dentists (22). Likewise, multiple clinics and private offices emerged, not all owned by dentists, seeking to fill in geographic coverage and quality gaps, or to provide services not included in the PBS. Examples of such services include orthodontics and oral implantology, which became the main source of employment for most dentists.
Unfortunately, labor and contractual conditions given by these clinics and offices have been precarious, prevailing contracts in which the dentist is paid a percentage of the cost charged to the patient for clinical treatments, or contracts for services provided that allow employers to avoid paying worker's social security. Moreover, in both types of contracts, in many cases, dentists have to provide their instruments and materials to carry out their work, which can affect the quality of care provided to the patient; that is, the precariousness of both income and working conditions, and quality of life has been prevalent for many dentists (23-25).
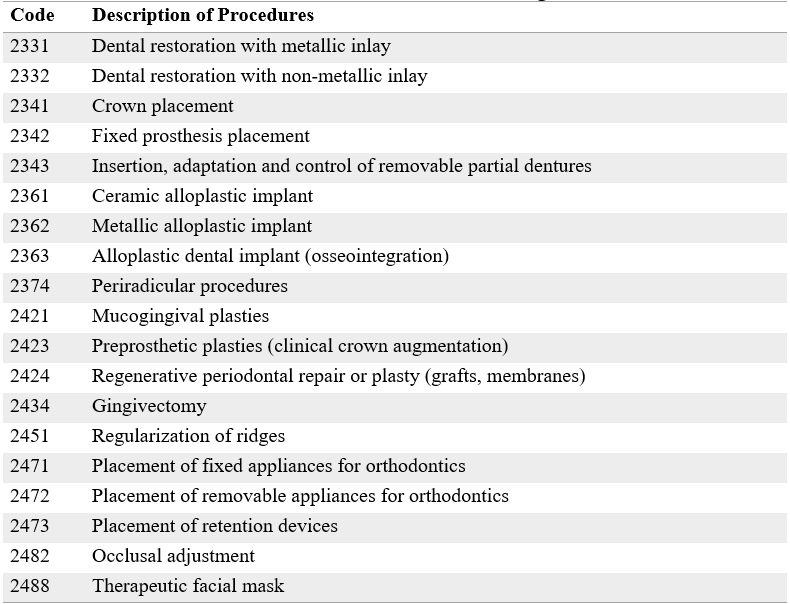
The contents of the PBS must be updated annually through the mechanisms established in the regulations and in accordance with scientific advances in services, technologies, and medications (7,9). However, the contents of oral health remained relatively stable for almost three decades, with only a few inclusions to those originally contemplated (26). This situation was modified with the issuance of Resolution 2292 of 2021 by the Ministry of Health and Social Protection (27). In said resolution, the oral health procedures that are financed by the Capitation Payment Unit (UPC) and that, therefore, must be provided by the EPSs and IPSs within the framework of the PBS, were expanded. The new procedures are listed in Table 1. As can be seen, procedures of fixed orthodontics and oral rehabilitation, in particular, osseointegration implants and associated periodontal activities were incorporated. Those procedures had been an important source of income for dentists specializing in such areas since they were not part of the PBS and were provided exclusively in private practice (25).
Additionally, the EPSs and IPSs that provide PBS services may be affected if the additional amounts paid by the SGSSS do not correspond to the costs they must incur to provide the new services to members. This can result in a decrease in coverage and the quality of care provided. Therefore, the inclusion of these procedures has generated wide discussion and disagreement among dentists, both general and specialists, suffering the possible impact on the liberal and institutionalized exercise that has been developing in the profession.
Therefore, some questions that merit analysis to establish possible future scenarios for the profession arise: Why are these procedures incorporated into the PBS? Can the costs of providing those procedures be supported by the Colombian government? How does professional practice, both private and institutionalized, change? Are these changes a threat or an opportunity for the future of the professional practice of dentistry? How to face and take advantage of the changes derived from the inclusion of these services? In short, this article seeks to answer the question: How can the inclusion of new oral health procedures in the PBS affect the practice of dentistry? For this reason, the aim was to analyze how the inclusion of new oral health procedures in the PBS affects the practice of dentistry.
TABLE 1
New Oral Health Procedures Included in the PBS according to Resolution 2292 of 2021
Source: Resolution 2292 of 2021 of the Health and Social Protection Ministry.
MATERIALS AND METHODS
This article presents the findings of a qualitative research through intrinsic document analysis of a case study (28). The study relied on the context and legal norms that govern the practice of dentistry in Colombia, within the SGSSS in Health framework and that have been established from the Political Constitution of 1991 to December 2021. The aim was to generate descriptions, identify patterns, explain causes, and propose solutions to the problems described. As tools for data collection, inductive observation, documents, records, legislation, and reflections with other professionals were used. The analysis of the information collected was conducted through a triangulation of structured data (29). The purpose was to analyze how the inclusion of new oral health procedures in the Health Benefits Plan (PBS) affects the practice of dentistry. Based on this, it is proposed to introduce some proposals that allow dentists to adapt to the change that this new scenario generates.
The documents were reviewed individually in analysis logs, identifying the parts that related to the practice of dentistry as units of analysis. Subsequently, we constructed open categories that helped us reveal potential meanings to begin to understand the essence of the research problem. Finally, we grouped them into explanatory categories of a selective type, which we called "central," in which the horizon of meaning of the texts was merged with the factual contexts of what dentists experienced in their daily professional practice (29). The resulting central categories became the basis to structure the findings.
Regarding the ethical and deontological aspects, the study did not include any experimentation with human beings (Declaration of Helsinki). Therefore, there was no risk, according to Resolution 8430 of 1993 of the Ministry of Health and Social Protection. All the data was anonymized to guarantee its confidentiality in compliance with the Habeas Data Law 1581 of 2012. Additionally, the use of citation rules in protection of copyright was guaranteed and no conflict of interest is reported for to conduct this project.
RESULTS
Inclusion of Oral Health Services as a Guarantee of the Right to Health
The first category of analysis that emerges relates to the guarantee of the right to health defined by Law 1751 of 2015, which establishes that, “The State shall adopt policies to ensure equal treatment and opportunities in access to promotional activities, prevention, diagnosis, treatment, rehabilitation and palliation for all people” (p. 1)(9).
As it can be inferred, the inclusion of new oral health procedures corresponds to the constant and progressive search that the Colombian State must perform in favor of the full enjoyment of the fundamental right to health by all the inhabitants of the national territory, without any distinction per ethnicity, gender, or socioeconomic status. This is also fully consistent with what is defined in article 13 of the Political Constitution, which states that, “All persons are born free and equal before the law, shall receive the same protection and treatment from the authorities, and shall enjoy the same rights, freedoms, and opportunities without any discrimination for reasons of sex, race, national or family origin, language, religion, political, or philosophical opinion” (p.2)(2).
From this point of view, the inclusion of new oral health procedures seeks to close the access gaps that populations, especially the most vulnerable, face when pursuing to restore their oral health. These procedures are very onerous and unattainable with most people’s income. In this regard, it is worth mentioning that, by 2021, 42 % of families had an income below the Current Minimum Legal Monthly Wage and 52 % of the country's population was food insecure (30). Despite the fact that the Colombian government implemented a monthly cash transfer worth $160,000 (US$40) to nearly four million of the poorest households (about 20 million people, that is, 40 % of the population of the country), called Solidarity Income (31).
Therefore, expanding the number of oral health services included in the PBS can be understood as an advance in the search for equity in health, although this fact alone does not guarantee effective access to care (32-33). For this, it is necessary that the installed capacity of oral health services corresponds to the demand that the population has for them. This requires an important planning and development of infrastructure exercise from which the country suffers (20,33). In addition, the only access restrictions to the included procedures can only be those that are established in Article 15 of Law 1751 of 2015:
-
a) Having as their main purpose a cosmetic goal, not necessarily related to the recovery or maintenance of a person’s functional or vital capacity;
-
b) Not existing scientific evidence on safety and clinical efficacy;
-
c) Not existing scientific evidence on clinical effectiveness;
-
d) Use not being authorized by the competent authority;
-
e) Being in experimentation phase;
-
f) Having to be performed abroad (9).
Of the restrictions listed above, only the first one is pertinent to the topic under discussion, since the other five should have already been afforded by having the procedures provided previously and charged to budget ceilings for care services that are not covered by the UPC, as defined in article 240 of law 1955 of 2019 (34). Therefore, the decision to provide or not a dental treatment with charge to the UPC will be the clinical criteria of the treating dentist, who will establish whether the requested care is functional or aesthetic. In this way, the autonomy of the professional takes on great importance, which is consistent with the provisions of Laws 1164 of 2007 (35), 1438 of 2011 (7) and 1751 of 2015 (9), as well as their professional ethical and deontological exercise framed in Law 35 of 1989 (14).
New Oral Health Inclusions and Their Impact on the SGSSS
The second category of analysis relates to the impacts the new inclusions may have on the country’s health care system. In this regard, the first doubt is about how it affects the financial sustainability of the system; In this sense, the Ministry of Health and Social Protection, through Resolution 2381 of 2021 (36), increased the average UPC of the contributory regime by 5.42 %, which represents going from CO$938,826 (US$213) in 2021 to CO$1,109,221.20 (US$252) in 2022. Likewise, the UPC of the subsidized regime increased 6.33 %, going from CO$872,496 (US$198) in 2021 to CO$964,807.20 (US$219) in 2022. These values, according to what was expressed by the Ministry, already include an increase of 12.73 % in the contributory regime and 4.25 % in the subsidized regime, which are precisely the ones with which the new procedures are financed as charges to the UPC, among which are those of oral health.
At the time of writing this article, the Ministry of Health and Social Protection had not published the frequency of use and historical indicators with which the calculations that led to the aforementioned increase were made. Simply, it has been limited to reporting that it was done based on the data on the use of the budget ceiling for the attention of non-PBS services by the EPSs in previous periods (37). In this sense, the Ministry argues that there is no new financial burden for the system, but rather a transfer of resources from the maximum budgets for non-PBS to the UPCs of the two regimes. In other words, it must be assumed that the oral health procedures included in the UPCs were already provided by the EPSs charged to the budget ceiling, an affirmation that generates doubts and uncertainty about the impact that their implementation will have on access, opportunity, security, and continuity of the treatments, especially when the frequencies of use of a service or procedure are not the same if it is required as non-PBS, given the existing administrative barriers to obtain it (My Prescription - MIPRES, rights protection petition) as when it is done by be part of the PBS and can be accessed directly only through clinical indication (37). Additionally, the calculation of the increase in the UPC may present exclusion biases of the real number of users who require oral health care, since, in the last two years, the demand for outpatient health services was reduced as an effect of the mobility restrictions adopted as a strategy to control the Covid-19 pandemic (38).
Regulated Rates and Materialization of Access to New Oral Health Procedures by the EPSs
Derived from the above, a third category of analysis emerges, since, to materialize the real access of patients to treatments, the EPSs will see the need to structure within their service networks the guarantee of the provision of these new oral health procedures through their own or contracted IPSs. In the latter, it is where private offices and dental clinics would be articulated, offering procedures through care and contracting models that must be defined with the EPSs (7,9,39-40).
In this process, there are no minimum contracting rates for health services that are binding between EPSs and IPSs, despite the fact that the mandatory nature of their creation was established in Article 29 of Law 1164 of 2007 (35), and the existing ones are for reference. Thus, the contracting process between EPSs and dental offices and clinics, which is governed by the free-markets economic logic, factors such as information asymmetry can lead to dominant positions that end up defining who wins and who loses in the negotiations of exchange prices (12,41).
In this regard, we interviewed a dentist who owns an IPS that provides outpatient services included in the PBS to an EPS. This person stated that the impact that this measure will have on capitation is going to be enormous, since the increases made by an EPS are meager when compared to the potential demand for these new oral health services to be provided by the EPSs. As an example, the interviewee stated that, of the 100 % of the rate he receives for each affiliate he must attend under the capitation figure with the EPS, they spend 28 % on dental care. This does not include new procedures. The person was concerned about the increase or payment for individual procedures. These values highlight the high financial risk that the provider may face if the increase received for each capitated member does not manage to dilute the new costs that must be incurred to provide the oral health services listed in Resolution 2292 of 2021.
Information Asymmetries in Health Markets
To understand the origin of the tensions between insurers and providers, the fourth category of analysis is developed below, which refers to the asymmetry of information in health markets. Particularly, markets of health services are highly asymmetrical in favor of health service providers, who are expected to perfectly know the conditions, characteristics, and production costs of the services they offer, something that the patient can hardly know. Therefore, relationships between patient and clinician should be based on trust (11). However, if the provider breaks the trust by unjustifiably raising prices in pursuit of high profit margins, unbeknownst to the patient, this can be to the financial detriment of patients. The exchange prices would be above those that could be considered fair and would only be limited by the elasticity of demand to the factor price (12,41).
In other words, in a direct relationship between the health service provider and the patient, ethics and deontology play a preponderant role in avoiding information asymmetries against the patient. This, not being easily adjustable and monitored, constitutes a constant moral risk, especially, in the case of dentistry, when some sections of Law 35 of 1989, which governs the ethics of the Colombian dentist, were declared unenforceable, especially those that limited the use of advertising or competition with colleagues through fees (42-43).
Moral hazard can be understood as the inability to take what is believed to be the ethically appropriate or the correct course of action, including avoiding harm or damage, due to institutionalized obstacles. It is a psychological response to an experience of conflict or moral restraint, which is especially likely to occur during public health emergencies and in other situations when there are extreme resource limitations that affect patient care and the safety of health care workers (44). To avoid such a moral hazard, health systems incorporate mechanisms that regulate the exchange price by defining agents through which payments between the State and providers are made through the disbursement of premiums, capitations, and/or pre-established rates for services, materials, and medicines used in patient care.
Thus, the SGSSS establishes that the national government, through the ADRES, recognizes a premium for each one of the members of the EPSs: the UPC. Through it, the EPSs must guarantee the delivery of services, technologies, and medicines included in the PBS. Moreover, in theory, the EPSs should regulate that the exchange prices that providers charge for the care required by their affiliates are fair. In other words, it would be understood that the EPSs, in addition to allowing access to those whose purchasing power prevents them from paying for the health care they require and, in general, reducing families' out-of-pocket expenses, have the function of reducing information asymmetries that pre-exist in the provider-patient relationship (1,4).
Now, in practice, what has happened is that EPSs, by concentrating information on health needs and the conditions in which care providers, have taken dominant positions by turning the asymmetry of information in their favor, against both health care providers and affiliates. This behavior has allowed them to impose rates and contracting conditions on health care providers, even below the costs of producing the services (this is especially the case in cities, since in small municipalities the provider, usually public, is the one who has the dominant position), which, in turn, health care providers end up transferring to users by reducing the opportunity and access to services. This affects the continuity of care and, in the medium term, their health condition.
For this reason, the definition of fixed rates for the payment of services constitutes one of the key elements that would avoid the dominant position of EPSs and that could guarantee that the provider of health services, among them the doctor's offices and clinics dental services, receive a payment that compensates for the costs incurred in providing the service (45). These fees could be per capita for first level care services and per event or prospective global payments, among other contracting figures, for services provided by specialists on an outpatient basis and/or by second and third level care clinics (7).
Another issue that generates a dominant position among the EPSs is that providers, likewise, seek to reduce their service production costs by reducing the wages of workers/contractors (whether they are professionals, technologists, technicians, or health care assistants), job precarization through per-service or per-procedure contracts, and/or personnel reduction. This entails greater workloads with the consequent results of work stress (Burnout Syndrome) that can culminate in adverse events and/or iatrogenesis affecting the health of patients (46).
Likewise, something that determines dominant positions, in this case between clinics and dental practices, is the generation of economies of scale that are achieved when services are sold by volume, which leads to the intensive and efficient use of equipment and supplies and to a full-load rate of health personnel. This is reflected in the reduction of service production costs, that is, the more that is produced, the lower the costs (47). This allows dental clinics to offer lower rates than those offered by dental offices, which results in them achieving dominant positions in the market.
In relation to economies of scale, it is evident that the regulations on quality, in particular, those referring to the authorization of health services, are aimed at favoring the creation of said economies. This occurs because the required infrastructure and equipment are clearly aimed at producing oral health services in large institutions, such as clinics, and not in small clinics (48-49). The purpose is to achieve greater productivity and efficiency in the use of SGSSS resources. To avoid this adverse selection and counteract this access barrier, the need arises for small practices to associate.
Labor Dignity in the Practice of Dentistry
As a fifth category of analysis, the need to establish decent hiring conditions appears. They include the elimination of contracts for the provision of services or procedures, that is, all health personnel must be hired with employment contracts, which makes it easier to define work schedules that reduce the risk of work stress and avoid transferring costs from employers to workers (22).
Particularly, in the hiring of dentists, job insecurity has spread to the point that most professionals are hired for the provision of services or procedures. They have been obliged to bring their own instruments, equipment and, in some cases, materials. This becomes a kind of subsidy that professionals make to the utility of the employer (10). This happens mainly in private clinics that have become the main sources of employment for the profession (23).
As a result, job dissatisfaction is high, a complaint that, in a study conducted in Cartagena Colombia, men expressed much more than women, as well as singles and dentists with several years of professional practice. The causes of this dissatisfaction include factors such as low pay and long working hours, mostly over eight hours a day, which led the study participants to perceive a divergence between the expectations they had when they entered the labor market and the factual reality experienced (24-25).
In the case of the oral health services of the IPSs that attend PBS patients, the situation is different; In IPSs, employment and service contracts are used (mainly for general dentists), which, from the point of view of remuneration, is more stable for the dentist. However, they are affected by the high volumes of patients that they must attend in extremely short consultation times, and which includes both clinical care and administrative management. This burden generates work stress with the possible effects, again, on the quality of care provided to patients, all of this as a consequence of installed capacities and insufficient personnel to meet the demand for care of the affiliated population (20-22).
DISCUSSION
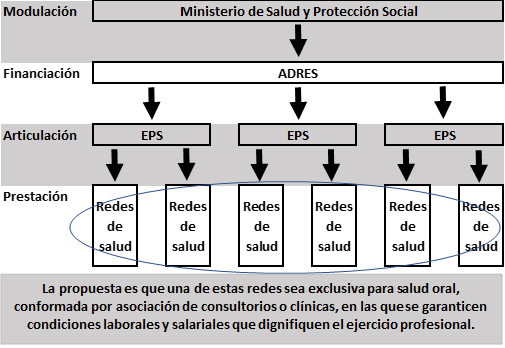
In this section, some scenarios are proposed that seek to guide possible strategies aimed at achieving better conditions for the practice of the dental profession (Figure 2).
Possible Scenarios for a Better Practice of Dentistry
The categories analyzed above allow us to identify the problems faced by the dental profession in Colombia both in clinical practice and in the relationship of the offices and clinics with each other, with the SGSSS, and with the team of human talent that works. Therefore, the question arises, how to turn these threats and weaknesses into opportunities to strengthen the dental profession? To do this, one must start by accepting that the transformations that the liberal practice of dentistry in Colombia has undergone, as a result of the gradual incorporation of the different specialties and advances in clinical procedures and technologies, is irreversible given the constitutional framework of the Social Welfare State in which guaranteeing the fundamental right to health prevails over any particular interest (2). Therefore, answering the question posed must be done within the existing regulatory framework.
Although the impact of the incorporation of new oral health services within the PBS on the volume of patients attending private consultations will not be immediate and will take at least a couple of years, it is clear that the liberal practice of dentistry must assume that its field of action has been limited and that trend will probably continue (10,20).
Therefore, the suggested way forward is associating, not only through guilds but also through clinics and offices, to eliminate the historical fragmentation that has existed, to a large extent, as a result of the individualism that has characterized dentistry at undergraduate training in Colombia. This implies, as a first goal, to comply with the development of strategies to transform the union culture as a foundation to the basic management processes to turn into an opportunity the institutionalization of clinical care of patients within the framework of the SGSSS (50). In pursuit of this purpose, it is necessary that guilds such as the Colombian Dental Federation, the Colombian College of Dentists, and specialist associations improve their credibility among dentists, who see them as distant, outside the day-to-day of the profession and, therefore, not very resolute in the face of the structural crisis that the profession is experiencing (Figure 2).
That said, the next strategy should be aimed at structuring oral health care networks made up of the articulation, coordination, and integration of dental clinics and offices under associative figures, in which each dentist co-owner becomes a partner to the extent possible of the infrastructures and services they provide. These oral health networks must guarantee the necessary installed capacity to allow timely care for patients referred by the EPSs with which they establish contracts. The strategy of integrated health networks is a proposal that has been promoted by the Pan-American Health Organization as a mechanism to avoid the fragmentation of health care systems and guarantee access, opportunity, and continuity of care for customers (51) (Figure 2).
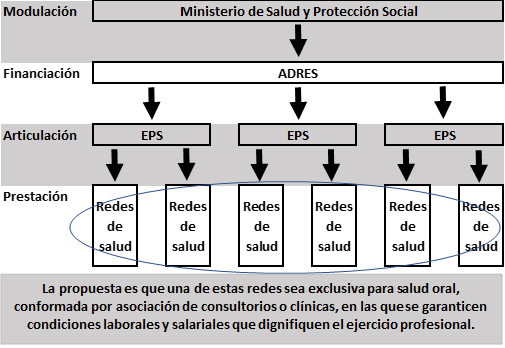 FIGURE 2
Diagram of the SGSSS and Proposal to Establish Oral Health Networks (in Spanish)
FIGURE 2
Diagram of the SGSSS and Proposal to Establish Oral Health Networks (in Spanish)
Additionally, and as a differentiating factor to give them a competitive advantage, all administrative and clinical processes must be conducted through ICTs that allow data digitalization and, ideally, automation through artificial intelligence, machine learning, and data mining. In this way, better results would also be achieved in diagnostic processes (52-53) and operational and personnel costs would be reduced in order to have a financial balance.
In addition, the success of this strategy will depend on the selection of hiring models that allow those who participate to obtain a sufficient income. Likewise, administrative and clinical management models must be established that achieve the maximum use of infrastructures, conducting clinical care under ethical principles and that guarantee the quality of care required by patients. Furthermore, the management of centralized purchases of supplies, instruments, and equipment should be included to reduce costs and develop information systems that serve as a core element for management and decision-making.
All of the above must be accompanied by the creation of a clinical care model that is based on disease prevention and early, timely, and continuous intervention of oral pathologies that afflict the patient. This should be complemented by the use of technological resources that allow accompanying clinical work and monitoring patients through telehealth, taking advantage of new applications for mobile devices and software that facilitate permanent contact with patients (54).
For this purpose, it will be an imperative that the type of contract that oral health networks must establish with the EPSs is capitation, which must be negotiated, first, as a percentage of the UPC and, second, requiring that the assigned population groups remain constant for at least five years, in order to give them a cohort-type clinical management that guarantees positive results in the epidemiological profile of oral health.
The following strategy necessarily goes through the strengthening of the power of negotiation and demanding the Ministry, state/department health secretariats, and EPSs the definition of: 1) fair rates, that is, that guarantee the recovery of costs and expenses involved in the production of oral health services that allow the proper management of oral health networks; 2) base salaries for contracting dentists by health service providers, including oral health networks, especially for general dentists who should become the pillar of the care model; and, 3) the pressure on EPSs so that oral health services are contracted with oral health networks consisting of offices and clinics owned by dentists.
CONCLUSIONS
In Colombia, the liberal exercise of dentistry will probably be increasingly limited given the progress of the guarantee of the fundamental right to health in compliance with the Social Welfare State promulgated in Article 1 of the Political Constitution. This can lead to access for all the inhabitants of the national territory to health services and procedures with relevant and safe technologies, without these implying direct out-of-pocket expenses, but instead being financed through general taxation and parafiscal payroll taxes.
For this reason, foreseeing the future of clinical practice necessarily implies thinking of scenarios in which, surely, institutional practice is the basis. Therefore, a cultural change from individualistic practice to associative collaboration will be required, both in the creation of oral health networks as well as the guild level as the essence of the demands from the profession to State institutions and private agents that are part of the SGSSS.
Finally, although there has always been reluctance, it will be increasingly imperative that the management of clinics requires training in health administration and management, as well as the incorporation of ICTs, since these, with high probability, will be the basis to guarantee health care in an ethical manner, quality, and costs that can make the existence of clinics and doctor's offices viable based on the rates at which they contract with the EPSs.
RECOMMENDATIONS
The findings presented in this article are primarily aimed at providing inputs to guilds in the health sector to conduct prospective exercises that help to dignify the practice of dentistry in institutional contexts and to defend the working and salary conditions of the profession.
Likewise, these findings are expected to be useful for the formulation of public policies, particularly those related to oral health, at the national and territorial levels. Likewise, they can contribute to the debate on the future of the practice of dentistry in Latin American regional contexts and even in countries where oral health is being provided in an institutionalized manner by the State through security or social protection systems. Also, the proposed scenarios can be useful for the planning of oral health services by insurers and providers of this service, whether public or private.
Finally, it would be expected that, to complement this research, others will aim at evaluating the quality of life of dentists under the current conditions in which the profession is practiced in Colombia. Additionally, it would be desirable if further research established the real costs and the implications that comprehensive oral health care for the entire population has for the Colombian health system, in order to establish the funding that is required to achieve such a broad and important goal for the well-being of the Colombian society.
References
1. República de Colombia. Ley 100 de 1993, por la cual se crea el sistema de seguridad social integral y se dictan otras disposiciones. Bogotá, Colombia: Congreso de la República; 1993.
2. Asamblea Nacional Constituyente. Constitución Política de la República de Colombia. Bogotá, Colombia: 1991.
3. Londoño de la Cuesta JL, Frenk J. Pluralismo Estructurado: Hacia un modelo innovador para la reforma de los sistemas de salud en América Latina. Documento de trabajo 353. Washington, DC: Banco Interamericano de Desarrollo; 1997
4. República de Colombia. Ley 1753 de 2015. por la cual se expide el Plan Nacional de Desarrollo 2014-2018 “Todos por un nuevo país”. Bogotá, Colombia: Congreso de la República; 2015.
5. República de Colombia. Decreto 064 de 2020. Por el cual se modifican los artículos 2.1.3.11, 2.1.3.13, 2.1.5.1, 2.1.7.7, 2.1.7.8 y 2.1.3.17, y se adicionan los articulas 2.1.5.4 y 2.1.5.5 del Decreto 780 de 2016, en relación con los afiliados al régimen subsidiado. Bogotá, Colombia: Presidencia; 2020.
6. Jiménez-Barbosa WG. Colombia y Costa Rica: enfoques de políticas en salud y resultados en el bienestar. Cienc Tecnol Salud Vis Ocul. 2009; (2): 167-178. https://doi.org/10.19052/sv.1068
7. República de Colombia. Ley 1438 de 2011, por medio de la cual se reforma el Sistema General de Seguridad Social en Salud y se dictan otras disposiciones. Bogotá, Colombia: Congreso de la República; 2011.
8. Corte Constitucional de Colombia. Sentencia T-760 de 2008. Bogotá, Colombia: 2008.
9. República de Colombia. Ley Estatutaria 1751 de 2015. Por medio de la cual se regula el derecho fundamental a la salud y se dictan otras disposiciones. Bogotá, Colombia: Congreso de la República; 2015.
10. Jaramillo G, Gómez GM. Efectos de la ley 100 sobre el campo de estudio y el quehacer de los profesionales de la salud: la práctica odontológica y su caso. Rev Fac Odontol Univ Antioq. 2006; 18(1): 95-102.
11. Arrow K. Uncertainty and the welfare economics of medical care. Am Econ Rev. 1963; 53(5): 941-973.
12. Córdoba Sánchez CI. Asimetría de información en el mercado de la salud en Colombia. Investig Enferm Imagen Desarrollo. 2005; 7(1-2): 48-59.
13. Cano Plata EA, Cano Plata CA. Los contratos, las asimetrías de la información en salud, el riesgo moral y la selección adversa. Rev Escuela de Admin Negocios. 2009; 67: 5-20.
14. República de Colombia. Ley 35 de 1989. Sobre ética del odontólogo colombiano. Bogotá, Colombia: Congreso de la República; 1989.
15. Ministerio de Salud. Decreto 654 de 1974, por el cual se establece la organización básica de la Dirección del Sistema Nacional de Salud. Bogotá, Colombia; 1974.
16. República de Colombia. Decreto 56 de 1975. Por el cual se sustituye el Decreto-ley número 654 de 1974 y se dictan otras disposiciones. Bogotá, Colombia: Presidencia; 1975.
17. Bran Piedrahita L, Valencia Arias A, Palacios Moya L, Gómez Molina S, Acevedo Correa Y, Arias Arciniegas C. Barreras de acceso del sistema de salud colombiano en zonas rurales: percepciones de usuarios del régimen subsidiado. Hacia Promoc Salud. 2020; 25(2): 29-38.
18. Rodríguez-Paez FG, Jiménez-Barbosa WG, Jiménez-González CA, Coral-Córdoba ÁE, Ramírez-Solano PC, Ramos-Navas NR. Efecto de las barreras de acceso sobre la asistencia a citas de programa de control prenatal y desenlaces perinatales. Rev Gerenc Polit Salud. 2014; 13(27): 212-227. http://dx.doi.org/10.11144/Javeriana.rgyps13-27.ebas
19. Restrepo-Zea JH, Silva-Maya C, Andrade-Rivas F, VH-Dover R. Acceso a servicios de salud: análisis de barreras y estrategias en el caso de Medellín, Colombia. Rev Gerenc Polít Salud. 2014; 13(27): 242-265. https://doi.org/10.11144/Javeriana.rgyps13-27.assa
20. Otálvaro Castro GJ, Zuluaga Salazar SM, Jaramillo Delgado G, Ternera Pulido JH, Sandoval Valencia S. Políticas de salud bucal en Colombia. Tendencias y puntos críticos para la garantía del derecho a la salud. Univ Odontol. 2019; 38(80). https://doi.org/10.11144/Javeriana.uo38-80.psbc
21. Agudelo-Suárez AA, Alzate-Urrea S, López-Vergel F, López-Orozco C, Espinosa-Herrera É, Posada-López A, Meneses-Gómez, EJ. Barreras y facilitadores de acceso a los servicios de salud bucal para la población adulta mayor atendida en la red pública hospitalaria de Medellín, Colombia. Rev Gerenc Polit Salud. 2014; 13(27): 181-199. http://dx.doi.org/10.11144/Javeriana.rgyps13-27.bfas
22. Jaramillo-Delgado GH, Marín-Flórez MJ, Cadavid-Berrio JP, Burgos-Amaya E, Osorio-Quintero MA, Velásquez-Benítez JA. Situación laboral de odontólogos egresados de la Universidad de Antioquia antes y durante la pandemia por la COVID-19, periodo 2015(1)-2019(2). Acta Odontol Colomb. 2021; 11(2): 86-101. http://dx.doi.org/10.15446/aoc.v11n2.94781
23. Donatres Giraldo JA, Rojas Amador MA, Jiménez Barbosa WG. Calidad de vida de los odontólogos en Colombia. Revisión exploratoria de la literatura. Univ Odontol. 2017; 36(76). https://doi.org/10.11144/Javeriana.uo36-76.cvoc
24. Romero-Polo JA, Mercado-Pacheco A, Díaz-Cárdenas S, de la Valle-Archibold M. Satisfacción laboral y condiciones laborales en odontólogos de Cartagena de Indias-Colombia. Arch Med (Manizales). 2021. 21(1): 138-149. https://doi.org/10.30554/archmed.21.1.3864.2021
25. Betancur Herrera HA, Franco Aguirre JQ, Sánchez Garzón J, Ochoa Acosta EM. Condiciones laborales y satisfacción de los graduados del programa de Ortodoncia, Universidad Cooperativa de Colombia. Estudio exploratorio. CES Odontol. 2021; 34(2): 107-122. https://doi.org/10.21615/cesodon.5719
26. Ministerio de Salud y Protección Social. Resolución 2481 de 2020, por la cual se actualizan integralmente los servicios y tecnologías de salud financiados con recursos de la Unidad de Pago por Capitación (UPC). Bogotá, Colombia; 2020.
27. Ministerio de Salud y Protección Social. Resolución 2292 de 2021, por la cual se actualizan los servicios y tecnologías de salud financiados con recursos de la Unidad de Pago por Capitación (UPC). Bogotá, Colombia; 2021.
28. Hernández Sampieri R, Fernández Collado C, Baptista Lucio P. Metodología de la investigación. 6ª. ed. México: McGraw-Hill; 2014.
29. Strauss A, Corbin J. Bases de la investigación cualitativa: técnicas y procedimientos para desarrollar la teoría fundamentada. 1ª. ed. español. Medellín, Colombia: Universidad de Antioquia; 2012.
30. Programa Mundial de Alimentos (PMA). VAM Bulletin #1. Análisis de la seguridad alimentaria. Roma, Italia: PMA; Febrero 2010.
31. Ministerio de Hacienda y Crédito Público. Decreto Legislativo 518 de 2020, por el cual se crea el Programa Ingreso Solidario para atender las necesidades de los hogares en situación de pobreza y vulnerabilidad en todo el territorio nacional, en el marco del Estado de Emergencia. Bogotá, Colombia: el Ministerio; 2020.
32. Sen A. ¿Por qué la equidad en Salud? Rev Panam Salud Publica/Pan Am J Public Health. 2002; 11(5-6): 302-309.
33. Rocha-Buelvas A. Análisis sobre el acceso a los servicios de la salud bucal: un indicador de equidad. Rev Gerenc Polit Salud. 2013; 12(25): 96-112.
34. República de Colombia. Ley 1955 de 2019, por el cual se expide el Plan Nacional de Desarrollo 2018-2022. “Pacto por Colombia, Pacto por la Equidad”. Bogotá, Colombia: Congreso de la República; 2019.
35. República de Colombia. Ley 1164 de 2007, por la cual se dictan disposiciones en materia del Talento Humano en Salud. Bogotá, Colombia: Congreso de la República; 2007.
36. Ministerio de Salud y Protección Social. Resolución Número 2381 de 2021 por la cual se fija el valor anual de la Unidad de Pago por Capitación - UPC que financiará los servicios y tecnologías de salud de los Regímenes Contributivo y Subsidiado para la vigencia 2022. Bogotá, Colombia: el Ministerio; 2021.
37. Dirección de Regulación de Beneficios, Costos y Tarifas del Aseguramiento en Salud (DRBCTAS). Respuesta a observaciones proyecto de resolución actualización de servicios y tecnologías en salud con cargo a la UPC - Procedimientos odontológicos - Bogotá, Colombia: DRBCTAS; 2021.
38. República de Colombia. Decreto 457 de 2020, por el cual se imparten instrucciones en virtud de la emergencia sanitaria generada por la pandemia del coronavirus COVID-19 y el mantenimiento del orden público. Bogotá, Colombia: la Presidencia; 2020.
39. República de Colombia. Ley 715 de 2001, por la cual se dictan normas orgánicas en materia de recursos y competencias de conformidad con los artículos 151, 288, 356 y 357 (Acto Legislativo 01 de 2001) de la Constitución Política. Bogotá, Colombia: Congreso de la República; 2001.
40. Barragán Bechara C, Riaño Casallas MI, Martínez M. Redes integradas de servicios de salud: hacia la construcción de un concepto. Univ Salud. 2012; 14(2): 186-196.
41. Bardey D. Competencia en el sector de la salud: énfasis en el caso colombiano. Coyuntura Econ Investig Econ Soc. 2013; XLIII (2): 17-52.
42. Corte Constitucional de Colombia. Sentencia C-355/94, propaganda de Servicios Profesionales/Ética-Violaciones. Bogotá, Colombia: la Corte; 1994.
43. Corte Constitucional de Colombia. Sentencia C-537/05. Bogotá, Colombia: la Corte; 2005.
44. Canadian Medical Association. COVID-19 and moral distress; 2021. Retrieved: 7 March 2022. https://www.cma.ca/sites/default/files/pdf/Moral-Distress-E.pdf
45. Bardey D, Castaño RA. La regulación de tarifas en el sector de la salud en Colombia. Rev Econ Inst. 2007; 9(17): 347-357.
46. Fajardo-Lazo J, Mesa-Cano IC, Ramírez-Coronel AA, Rodríguez Quezada FC. Professional burnout syndrome in health professionals. Arch Venez Farmacol Terapeutica. 2020; 40(3): 1-7. https://doi.org/10.5281/zenodo.5038655
47. Keith J, Prior D. Scale and scope economies in Mexican private medical units. Salud Publica Mex. 2014; 56(4): 348-354.
48. República de Colombia. Decreto 780 de 2016, por medio del cual se expide el Decreto Único Reglamentario del Sector Salud y Protección Social. Bogotá, Colombia: Presidencia; 2016.
49. Ministerio de Salud y Protección Social. Resolución 3100. por la cual se definen los procedimientos y condiciones de inscripción de los prestadores de servicios de salud y de habilitación de los servicios de salud. Bogotá, Colombia: El Ministerio; 2019.
50. Asociación Gremial Odontológica de Antioquia. Carta al Gremio Odontológico de Colombia. 14 mayo 2020.
51. Organización Panamericana de la Salud (OPS). Redes integradas de servicios de salud: conceptos, opciones de política y hoja de ruta para su implementación en las Américas. Washington, DC: OPS; 2010.
52. Ameli N, Gibson MP, Khanna A, Howey M, Lai H. An application of machine learning techniques to analyze patient information to improve oral health outcomes. Front Dent Med. 2022; 3(833191): 1-11. https://doi.org/10.3389/fdmed.2022.833191
53. Mao-Lei S, Yun L, Guomin L, Dan C, Ali Asghar H, Wen-Yuan J, Xuan J, Huiling C, Yungang L. Application of machine learning to stomatology. IEEE Access. 2020; 8: 184360-184374.
54. Jiménez-Barbosa WG, Acuña-Gómez S. Avances en telesalud y telemedicina: estrategia para acercar los servicios de salud a los usuarios. Acta Odontol Colomb. 2015; 5(1): 101-115.
Notes
*
Original research.
Author notes
Correspondence: wilsong.jimenezb@utadeo.edu.co; jsacuna1@fucsalud.edu.co
Additional information
How to cite this article: Jiménez-Barbosa WG, Acuña Gómez JS. Inclusion of Oral Health Procedures Funded by the Colombian Government and Possible Effects on Dentistry’s Practice. Univ Odontol. 2022; 41. https://doi.org/10.11144/Javeriana.uo41.iohp