Resumen
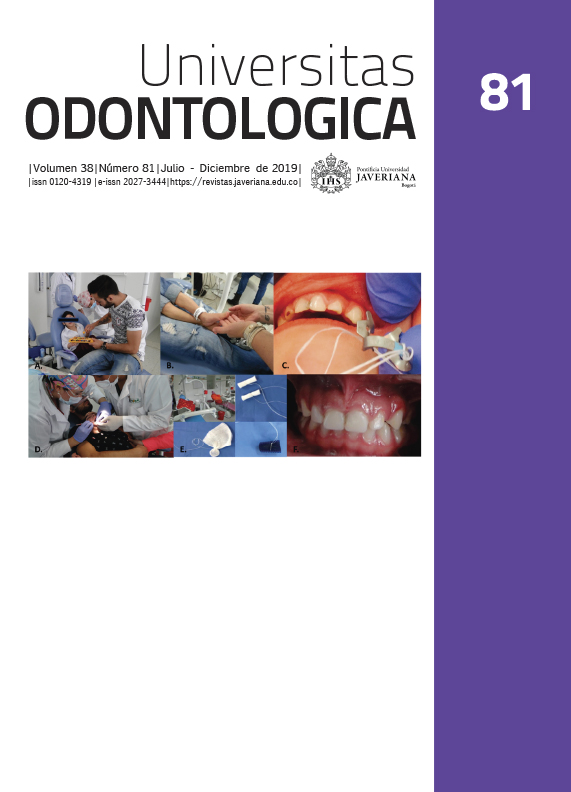
Antecedentes: Una de las alteraciones del neurodesarrollo en los niños con <1500 g de peso al nacer es la parálisis cerebral espástica (PCE) que se asocia con microcefalia, epilepsia, discapacidad intelectual y retraso global del desarrollo. Objetivo: Describir el manejo estomatológico de un niño con cuadriparesia espástica. Descripción del caso: Para publicar este caso, se obtuvo autorización en consentimiento informado. El paciente era visto por un equipo multidisciplinario desde temprana edad pero solo ingresó al servicio de Estomatología Pediátrica de la Fundación Hospital Pediátrico de la Misericordia de Bogotá cuando tenía de 3 años 7 meses. El niño tenía antecedentes de prematuridad: 28 semanas; peso: 925 g; talla: 34 cm: perímetro cefálico: 25 cm. Diagnósticos sistémicos: PCE, microcefalia, epilepsia, discapacidad intelectual grave y retraso global del desarrollo. Examen físico: 9 kg de peso, 52 cm de estatura y 34 cm de perímetro cefálico. Examen extraoral: dolicocéfalo, perfil convejo, micrognatismo mandibular, apertura bucal 1,5 cm. Examen intraoral: caries de infancia temprana. Se realizó atención odontológica integral con retiro de focos sépticos, motivación e instrucción en higiene oral. Conclusión: El equipo multidisciplinario para la atención de niños prematuros con alteraciones del neurodesarrollo, microcefalia y bajo peso al nacer debe contar con la presencia del(la) estomatólogo(a) u odontólogo(a) pediatra para iniciar procesos de promoción y prevención en salud bucal individualizados para evitar caries de infancia temprana y mejorar la calidad de vida.
2. Robaina Castellanos G, Ruiz Tellachea Y, Domínguez Dieppa F, Roca Molina MC, Riesgo Rodríguez S, Berdayes Millián JD. Neurodesarrollo en recién nacidos ventilados con menos de 1500 gramos. Rev Cub Pediatr. 2015; 72(4): 267-74.
3. Agency for Clinical Innovation. Management of cerebral palsy in children: a guide for allied health professionals. (GL2018_006). North Sydney, Australia; New South Wales Ministry of Health; 2018. Available at: https://www1.health.nsw.gov.au/pds/ActivePDSDocuments/GL2018_006.pdf
4. Malagón Valdez J. Parálisis cerebral. Medicina (Buenos Aires). 2015; 67(6): 586-92.
5. Ardila S, Espinosa E. Caracterización clínica y radiológica de pacientes pediátricos con malformaciones de corteza cerebral en dos hospitales de Bogotá periodo 2007-2010. Bogotá, Colombia: Universidad Militar Nueva Granada; 2010.
6. Nazer H J, Cifuentes O L. Malformaciones congénitas en Chile y Latino América: Una visión epidemiológica del ECLAMC del período 1995-2008. Rev Med Chile. 2011; 139(1): 72-8.
7. Pachajoa H, Ariza Y, Isaza C, Méndez F. Defectos congénitos mayores en un hospital de tercer nivel en Cali, Colombia 2004-2008. Rev Salud Publica (Bogotá). 2011; 13(1): 152-62.
8. Abanto J, Ortega AO, Raggio DP, Bönecker M, Mendes FM, Ciamponi AL. Impact of oral diseases and disorders on oral-health-related quality of life of children with cerebral palsy. Spec Care Dentist. 2014 Mar-Apr; 34(2): 56-63.
9. Barrionuevo NL, Solís FF. Anomalías dentó maxilares y factores asociados en niños con parálisis cerebral. Rev Chil Pediatr. 2008; 79(3): 272-80.
10. Sehrawat N, Marwaha M, Bansal K, Chopra R. Cerebral palsy: a dental update. Int J Clin Pediatr Dent. 2014; 7(2): 109-18.
11. National Guidance Alliance (UK). Cerebral palsy in the under-25s: assessment and management. London, UK: National Institute for Health and Care Excellence. 2017 Jan. Available at: https://www.ncbi.nlm.nih.gov/books/NBK419326/
12. Martí Herrero M, Cabrera López JC. Macro- y microcefalia. Trastornos del crecimiento craneal. (Protocolos diagnósticos y terapéuticos en Pediatría). Madrid, España: Asociación Española de Pediatría; 2008. Disponible en: https://www.aeped.es/sites/default/files/documentos/25-macromicrocefalia.pdf
13. Organización Mundial de la Salud (OMS). Patrones de crecimiento infantil. Puntuación Z niños OMS. Ginebra, Suiza: OMS; 2018.
14. López Rodríguez YN. Antropometría craneofacial en niños de 0 a 4 años. Una perspectiva Bayesiana. Bogotá, Colombia: Universidad Nacional de Colombia, Repositorio Institucional; 2015. Disponible en: https://repositorio.unal.edu.co/handle/unal/54052
15. Díaz AT. Estudio de la densidad ósea en niños y adolescentes con afectación moderada y severa por parálisis cerebral. (Tesis doctoral). Sevilla, España: Universidad de Sevilla; 2016. Disponible en: https://idus.us.es/xmlui/handle/11441/39821
16. Rodrigues Santos MTB, Guare RO, Celiberti P, Siqueira WL. Caries experience in individuals with cerebral palsy in relation to oromotor dysfunction and dietary consistency. Special Care Dent. 2009; 29(5): 198.
17. Santos MTBR, Manzano FS, Genovese WJ. Different approaches to dental management of self-inflicted oral trauma: oral shield, botulinum toxin type A neuromuscular block, and oral surgery. Quintessence Int. 2008 Feb; 39(2): e63-69.
18. Gutierrez GM, Siqueira VL, Loyola-Rodriguez JP, Diniz MB, Guaré RO, Ferreira AC, Santos MT. Effects of treatments for drooling on caries risk in children and adolescents with cerebral palsy. Med Oral Patol Oral Cir Bucal. 2019 Mar 1; 24(2): 204-10.
19. Bolaños-Sánchez J. Caries de aparición temprana en infantes con parálisis cerebral espástica: ventajas de usar el sistema internacional de detección y evaluación de caries ICDAS. KIRU. 2015 ene-jun; 12(1): 74-8.
20. Akhter R, Hassan NMM, Martin EF, Muhit M, Smithers-Sheedy H, Badawi N, Khandaker G. Caries experience and oral health-related quality of life (OHRQoL) of children and adolescents with cerebral palsy in a low-resource setting. BMC Oral Health. 2019; 19(1): 15.
21. Santos MT, Guare RO, Celiberti P, Siqueira WL. Caries experience in individuals with cerebral palsy in relation to oromotor dysfunction and dietary consistency. Spec Care Dentist. 2009 Oct; 29(5): 198-203.
22. Guideline on management of dental patients with special health care needs. Pediatr Dent. 2016 Oct 15; 38(5): 67-72.
23. Ministerio de Salud. Guía clínica. Salud oral integral para menores de 20 años en situación de discapacidad que requieren cuidados especiales en odontología. Santiago, Chile: Minsal; 2012.
24. Martínez H, Treviño M, Rivera G. Guía para el cuidado de la salud oral en pacientes con necesidad de cuidados especiales de salud en México. Revista ADM. 2011; LXVIII(5): 222-8.
25. Santacruz HDL, Molinar YH, Sandoval BEM, Berber MÁR, Delgadillo GT. Estrategias terapéuticas de calidad en odontopediatría: parálisis cerebral. Acta Pediatr Méx. 2019 ene 28; 40(1): 32-43.
26. Parakh A, Singh R, Bhat D, Kulkarni N, Fernandes G. A Mini review on cerebral palsy and its implications in dentistry. OBDS. 2018 dic 10; 01-7.
Esta revista científica se encuentra registrada bajo la licencia Creative Commons Reconocimiento 4.0 Internacional. Por lo tanto, esta obra se puede reproducir, distribuir y comunicar públicamente en formato digital, siempre que se reconozca el nombre de los autores y a la Pontificia Universidad Javeriana. Se permite citar, adaptar, transformar, autoarchivar, republicar y crear a partir del material, para cualquier finalidad (incluso comercial), siempre que se reconozca adecuadamente la autoría, se proporcione un enlace a la obra original y se indique si se han realizado cambios. La Pontificia Universidad Javeriana no retiene los derechos sobre las obras publicadas y los contenidos son responsabilidad exclusiva de los autores, quienes conservan sus derechos morales, intelectuales, de privacidad y publicidad.
El aval sobre la intervención de la obra (revisión, corrección de estilo, traducción, diagramación) y su posterior divulgación se otorga mediante una licencia de uso y no a través de una cesión de derechos, lo que representa que la revista y la Pontificia Universidad Javeriana se eximen de cualquier responsabilidad que se pueda derivar de una mala práctica ética por parte de los autores. En consecuencia de la protección brindada por la licencia de uso, la revista no se encuentra en la obligación de publicar retractaciones o modificar la información ya publicada, a no ser que la errata surja del proceso de gestión editorial. La publicación de contenidos en esta revista no representa regalías para los contribuyentes.