Resumen
Introducción: Los desenlaces neonatales adversos se asocian a un gran costo económico a los sistemas de salud. Existe una preocupación creciente por la relación directamente proporcional entre el número de sobrevivientes y las tasas de discapacidad de los recién nacidos prematuros. El objetivo fue describir la morbilidad y la mortalidad en recién nacidos menores de 32 semanas de edad gestacional y determinar los factores asociados. Materiales y métodos: Estudio de corte transversal con componente analítico, que incluyó todos los recién nacidos pretérmino menores de 32 semanas de edad gestacional, que nacieron entre enero de 2018 y diciembre de 2020 y que continuaron su seguimiento en el programa Madre Canguro de la misma institución. Resultados: Se identificaron 108 recién nacidos. Los principales desenlaces fueron displasia broncopulmonar con una frecuencia del 85,9% entre los sobrevivientes y una mortalidad global del 27,7%. Se resalta la gran fuerza de asociación entre el choque séptico y el fallecimiento (ORa=275; p= 0,004); en ese mismo sentido, la edad gestacional (ORa=83,3; p= 0,004). Conclusiones: La incidencia de DBP en los pretérminos menores de 32 semanas es alta, constituyendo la morbilidad más importante en este grupo, con una mortalidad global significativa asociada. En términos de mortalidad la probabilidad de morir en estos recién nacidos, está explicada por menor edad gestacional (<28 semanas), nivel de hemoglobina más bajo, mayor necesidad de transfusiones, y la presencia de choque séptico. Palabras claves: Morbilidad; Mortalidad; Pretérminos; Neonatos (Fuente DeCS).
REFERENCIAS BIBLIOGRÁFICAS
Vwalika B, Price JT, Rosenbaum A, Stringer JSA. Reducing the global burden of preterm births. Lancet Glob Health. 2019;7(4):e415.
Seethapathy J, Boominathan P, Uppunda AK, Ninan B. Changes in Auditory Brainstem Response in very preterm and late preterm infants. Int J Pediatr Otorhinolaryngol. 2019;121:88-94.
Frey HA, Klebanoff MA. The epidemiology, etiology, and costs of preterm birth. Semin Fetal Neonatal Med. 2016;21(2):68-73.
Tracy MK, Berkelhamer SK. Bronchopulmonary Dysplasia and Pulmonary Outcomes of Prematurity. Pediatr Ann. 2019;48(4):e148-e153.
Bancalari E, Claure N, Sosenko IR. Bronchopulmonary dysplasia: changes in pathogenesis, epidemiology and definition. Semin Neonatol. 2003;8(1):63-71.
Reiterer F, Scheuchenegger A, Resch B, Maurer-Fellbaum U, Avian A, Urlesberger B. Bronchopulmonary dysplasia in very preterm infants: Outcome up to preschool age, in a single center of Austria. Pediatr Int. 2019;61(4):381-387.
García Reymundo M, Hurtado Suazo JA, Calvo Aguilar MJ, et al. Recomendaciones de seguimiento del prematuro tardío [Follow-up recommendations for the late preterm infant]. An Pediatr (Engl Ed). 2019;90(5):318.e1-318.e8
Castro Carrasco, Pablo, & Barraza Rodríguez, Paulo. (2007). Diferencias Cerebrales en Prematuros y su Relación con el Desarrollo de sus Funciones Cognitivas. Terapia psicológica, 25(2), 183-188.
Brandt I, Sticker EJ, Höcky M, Lentze MJ. Transient abnormal neurologic signs (TANS) in a longitudinal study of very low birth weight preterm infants. Early Hum Dev. 2000;59(2):107-126.
Degos V, Loron G, Mantz J, Gressens P. Neuroprotective strategies for the neonatal brain. Anesth Analg. 2008;106(6):1670-1680.
Dogra MR, Katoch D, Dogra M. An Update on Retinopathy of Prematurity (ROP). Indian J Pediatr. 2017;84(12):930-936.
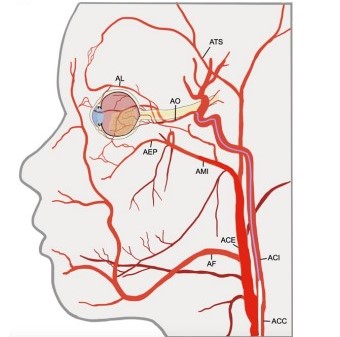
Giraldo M., Hurtado A., Donado J., Molina M. Epidemiología de la retinopatía del prematuro en Medellín, 2003-2008. Iatreia Vol. 24 (3): 250 - 258, 2011.
Multicenter trial of cryotherapy for retinopathy of prematurity. Preliminary results. Cryotherapy for Retinopathy of Prematurity Cooperative Group. Arch Ophthalmol. 1988;106(4):471-479.
Kiciński P, Kęsiak M, Nowiczewski M, Gulczyńska E. Bronchopulmonary dysplasia in very and extremely low birth weight infants - analysis of selected risk factors. Pol Merkur Lekarski. 2017;42(248):71-75.
Geary C, Caskey M, Fonseca R, Malloy M. Decreased incidence of bronchopulmonary dysplasia after early management changes, including surfactant and nasal continuous positive airway pressure treatment at delivery, lowered oxygen saturation goals, and early amino acid administration: a historical cohort study. Pediatrics. 2008;121(1):89-96.
Jiangsu Multicenter Study Collaborative Group for Breastmilk Feeding in Neonatal Intensive Care Units. Zhonghua Er Ke Za Zhi. 2019;57(1):33-39.
Tapia JL, Agost D, Alegria A, et al. Bronchopulmonary dysplasia: incidence, risk factors and resource utilization in a population of South American very low birth weight infants. J Pediatr (Rio J). 2006;82(1):15-20.
Chaw PS, Hua L, Cunningham S, et al. Respiratory Syncytial Virus-Associated Acute Lower Respiratory Infections in Children With Bronchopulmonary Dysplasia: Systematic Review and Meta-Analysis. J Infect Dis. 2020;222(Suppl 7):S620-S627.
Voynow JA. "New" bronchopulmonary dysplasia and chronic lung disease. Paediatr Respir Rev. 2017;24:17-18.
Instituto Nacional de Salud INS. Boletín epidemiológico semanal BES. Mortalidad Perinatal y Neonatal y Morbilidad Materna Extrema Neonatal. Colombia, 2020. www.ins.gov.co
Lehtonen L, Gimeno A, Parra-Llorca A, Vento M. Early neonatal death: A challenge worldwide. Semin Fetal Neonatal Med. 2017;22(3):153-160.
Pallás Alonso C, García González P, Jimenez Moya A, et al. Protocolo de seguimiento para el recién nacido menor de 1.500 g o menor de 32 semanas de edad gestación [Follow-up protocol for newborns of birthweight less than 1500 g or less than 32 weeks gestation]. An Pediatr (Barc). 2018;88(4):229.e1-229.e10.
Counsell SJ, Boardman JP. Differential brain growth in the infant born preterm: current knowledge and future developments from brain imaging. Semin Fetal Neonatal Med. 2005;10(5):403-410.
Bhutta AT, Cleves MA, Casey PH, Cradock MM, Anand KJ. Cognitive and behavioral outcomes of school-aged children who were born preterm: a meta-analysis. JAMA. 2002;288(6):728-737.
Di Fiore JM, MacFarlane PM, Martin RJ. Intermittent Hypoxemia in Preterm Infants. Clin Perinatal. 2019;46(3):553-565.
David K Coats, M D. Retinopathy of prematurity: Treatment and prognosis. UpToDate, 2020.
Sola A, Chow L, Rogido M. Retinopatía de la prematuridad y oxigenoterapia: una relación cambiante [Retinopathy of prematurity and oxygen therapy: a changing relationship]. An Pediatr (Barc). 2005;62(1):48-63.
Polin RA, Carlo WA; Committee on Fetus and Newborn; American Academy of Pediatrics. Surfactant replacement therapy for preterm and term neonates with respiratory distress. Pediatrics. 2014;133(1):156-163.
Hussain WA, Marks JD. Approaches to Noninvasive Respiratory Support in Preterm Infants: From CPAP to NAVA. Neoreviews. 2019;20(4):e213-e221.
Roberts D, Brown J, Medley N, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2017;3(3):CD004454.

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.
Derechos de autor 2021 antonio carlos puello avila, Edgar Felipe Laiseca Torres