Spasticity
##plugins.themes.bootstrap3.article.details##
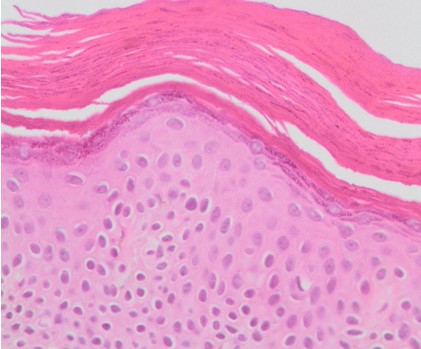
Spasticity is a motor disorder that forms part of the upper motor neuron syndrome and it is characterized by a speed-dependent increase in the tonic stretch reflex or muscle tone; accompanied by exaggerated myotendinous reflexes and hyperexcitability of the stretch reflex. It is frequently seen in patients with upper motor neuron syndrome secondary to various pathologies such as cerebrovascular attacks, spinal cord injuries, multiple sclerosis and cerebral palsy. A multidisciplinary and individualized approach is essential in the treatment of patients; which includes non-pharmacological, pharmacological, neurosurgical and orthopedic management. The present paper intends to carry out an updated non-systematic review on the history, epidemiology, pathophysiology, diagnosis and therapeutic approach to spasticity, both in the adult and pediatric population; as well as proposing a therapeutic algorithm.
Spasticity, Dystonia, Muscle hypertonia, Neuropharmacology, Upper motor neuron syndromeEspasticidad, Distonía, Hipertonía muscular, Neurofarmacología, Síndrome de motoneurona superior
1. Thilmann, AF; Burke, DJ; Rymer W. Spasticity and management. Springer Verlag; 1993.
2. Sherrington CS. Descerebrate rigidity and reflex coordination of movements. J Physiol. 1898;22(4):319–32.
3. Acevedo González JC. Espasticidad. Neurociencias en Colomb. 2001;9:133.
4. Feldman, R; Young, RR; Koella W. Spasticity, disordered motor control. Miami, FL; Chicago: Symposia Specialists ; Distributed by Year Book Medical Publishers; 1980.
5. Acevedo González JC. Definición y fisiopatología de la espasticidad. Neurociencias en Colomb. 2001;9:134–42.
6. Pandyan AD, Gregoric M, Barnes MP, Wood D, Van Wijck F, Burridge J, et al. Spasticity: clinical perceptions, neurological realities and meaningful measurement. Disabil Rehabil. 2005 Jan;27(1–2):2–6.
7. Bethoux F. Spasticity Management After Stroke: Stroke Spasticity Symptom management Outcome measures Rehabilitation. Phys Med Rehabil Clin NA [Internet]. 2015;26(4):625–39. Available from: http://dx.doi.org/10.1016/j.pmr.2015.07.003
8. Elbasiouny SM, Moroz D, Bakr MM, Mushahwar VK. Management of Spasticity After Spinal Cord Injury: Current Techniques and Future Directions. Neurorehabil Neural Repair. 2014;24(1):23–33.
9. Francisco GE, Mcguire JR. Poststroke Spasticity Management. Stroke. 2012;43(3):3132–6.
10. Vivancos-matellano F, Pascual-pascual SI, Nardi-vilardaga J, Miquel-rodríguez F. Guía del tratamiento integral de la espasticidad. Rev Neurol. 2007;45(6):365–75.
11. Acevedo Gonzalez, Juan Carlos; Pardo, Jorge Luis; Jimenez E. Secuelas espásticas de las enfermedades neurológicas. Acta Médica Colomb. 2000;25(2):75–83.
12. Graham L. Management of spasticity revisited. Age Ageing. 2013;42:435–41.
13. Trompetto C, Marinelli L, Mori L, Pelosin E, Currà A, Molfetta L, et al. Pathophysiology of Spasticity: Implications for Neurorehabilitation. Biomed Res Int. 2014
14. Cavorzin P Le. Espasticidad muscular: situación actual y perspectivas. Kinesiterapia- Med física. 2016;34(13):1–16.
15. Mayer NH. Clinicophysiologic Concepts of Spasticity and Motor Dysfunction in Adults with an Upper Motoneuron Lesion Syndrome : Positive and Negative. Muscle Nerve. 1997;1–13.
16. Ward AB. A literature review of the pathophysiology and onset of post-stroke spasticity. Eur J Neurol. 2012;19:21–7.
17. Sheean G. The pathophysiology of spasticity. Eur J Neurol. 2002;9:3–9.
18. Yelnik AP, Simon O, Bensmail D, Chaleat-valayer E, Decq P, Dehail P, et al. Drug treatments for spasticity. Ann Phys Rehabil Med. 2016;52(2009):746–56.
19. Acevedo González, Juan Carlos; Pardo Lang JL. Pautas de evaluación clínica para el manejo de la espasticidad. Neurociencias en Colomb. 2001;9:143–53.
20. Sheean G, Mcguire JR. Spastic Hypertonia and Movement Disorders : Pathophysiology , Clinical Presentation , and Quantification. PM R [Internet]. 2009;1(9):827–33. Available from: http://dx.doi.org/10.1016/j.pmrj.2009.08.002
21. Aloraini SM, Gäverth J, Yeung E, MacKay-Lyons M. Assessment of spasticity after stroke using clinical measures: a systematic review. Disabil Rehabil. 2015;37(25):2313–23.
22. Wade DT, Collin C. The Barthel ADL Index: a standard measure of physical disability? Int Disabil Stud. 1988;10(2):64–7.
23. Ghai A, Garg N. Spasticity – Pathogenesis , prevention and treatment strategies. Saudi J Anaesth. 2013;7(4).
24. Biering-Sorensen, F; Nielsen, JB;Klinge K. Review Spasticity-assessment: a review. Spinal Cord. 2006;44:708–22.
25. Strommen JA. Management of Spasticity from Spinal Cord Dysfunction. Neurol Clin NA [Internet]. 2013;31(1):269–86. Available from: http://dx.doi.org/10.1016/j.ncl.2012.09.013
26. Sindou M, Georgoulis G, Mertens P. Neurosurgery for Spasticity. Springer; 2014.
27. Smania N, Picelli A, Munari D, Geroin C, Ianes P, Waldner A, et al. Rehabilitation procedures in the management of spasticity. Eur J Phys Rehabil Med. 2010 Sep;46(3):423–38.
28. Dietz V, Sinkjaer T. Spasticity. Handb Clin Neurol. 2012;109:197–211.
29. Nl A, Le S, Deforge D. Treatment for spasticity in amyotrophic lateral sclerosis / motor neuron disease ( Review ). Cochrane Libr. 2012;(2).
30. Watanabe TK. Role of Oral Medications in Spasticity Management. PM R [Internet]. 2009;1(9):839–41. Available from: http://dx.doi.org/10.1016/j.pmrj.2009.07.014
31. Montané E, Vallano A, Laporte JR. Oral antispastic drugs in nonprogressive neurologic diseases A systematic review. Neurology. 2004;63:1357–64.
32. Acevedo Gonzalez JC. Tratamiento neuroquirúrgico de la espasticidad. Neurociencias en Colomb. 2006;14(2).
33. Obrien, DF; Park T. A review of orthopedic surgeries after selective dorsal rhizotomy. Neurosurg Focus. 2006;21(2):1–8.
34. Olver J, Esquenazi A, Fung VSC, Singer BJ, Ward AB. Botulinum toxin assessment , intervention and aftercare for lower limb disorders of movement and muscle tone in adults : international consensus statement. 2010;17:57–73.
35. Patel DR, Neelakantan M, Pandher K, Merrick J. Cerebral palsy in children: a clinical overview. Transl Pediatr. 2020;9(1).
36. AJL W. Review of electrical stimulation, botulinum toxin, and their combination for spastic drop foot. J Rehabil Res Dev [Internet]. 2013;50(3):315–26. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L369093355
37. Rodgers H, Shaw L, Price C, van Wijck F, Barnes M, Graham L, et al. Study design and methods of the BoTULS trial: a randomised controlled trial to evaluate the clinical effect and cost effectiveness of treating upper limb spasticity due to stroke with botulinum toxin type A. Trials. 2008 Oct;9:59.
38. Gracies J-M. Physiological effects of botulinum toxin in spasticity. Mov Disord. 2004 Mar;19 Suppl 8:S120-8.
39. Acevedo González, Juan Carlos ; Acevedo OL. Manejo integral de la espasticidad: Procedimientos objetivos orientados a mejorarla funcionalidad, la calidad de vida y a evitar el deterioro ortopédico. Médica Sanitas. 2003;6(4).
40. Acevedo Gonzalez JC. Manejo neuroquirúrgico de la espasticidad. Neurociencias en Colomb. 2001;9:181–90.
41. Furr-Stimming E, Boyle AM, Schiess MC. Spasticity and intrathecal baclofen. Semin Neurol. 2014 Nov;34(5):591–6.
42. Acevedo Gonzalez, Juan Carlos; Mayorga JD. Papel de la neurocirugía en el desarrollo de las técnicas de infusión continua de medicamentos intratecales R.D. Penn y J.R. Kroin. Rev Of la Asoc Colomb para el Estud del Dolor. 2008;3(4).
43. Ivanhoe CB, Francisco GE, McGuire JR, Subramanian T, Grissom SP. Intrathecal baclofen management of poststroke spastic hypertonia: implications for function and quality of life. Arch Phys Med Rehabil. 2006 Nov;87(11):1509–15.
44. Hsieh, JC; Penn R. Intrathecal baclofen in the treatment of adult spasticity. Neurosurg Focus. 2006;21(2):1–6.
45. Overgard TM, Kjaersgaard-Hansen L, Soe M, Illum NO. Positive experience with intrathecal baclofen treatment in children with severe cerebral palsy. Dan Med J. 2015 Jan;62(1):A4999.
46. Gray N, Morton RE, Brimlow K, Keetley R, Vloeberghs M. Original article Goals and outcomes for non ambulant children receiving continuous infusion of intrathecal baclofen. Eur J Paediatr Neurol [Internet]. 2012;44(0):1–6. Available from: http://dx.doi.org/10.1016/j.ejpn.2012.01.003
47. Natale M, Mirone G, Rotondo M, Moraci A. Intrathecal baclofen therapy for severe spasticity : Analysis on a series of 112 consecutive patients and future prospectives. Clin Neurol Neurosurg [Internet]. 2011; Available from: http://dx.doi.org/10.1016/j.clineuro.2011.10.046
48. Sindou M, Mertens P, Wael M. Microsurgical DREZotomy for pain due to spinal cord and/or cauda equina injuries: long-term results in a series of 44 patients. Pain. 2001 May;92(1–2):159–71.
49. Sitthinamsuwan B, Nunta-Aree S. Ablative neurosurgery for movement disorders related to cerebral palsy. J Neurosurg Sci. 2015 Dec;59(4):393–404.
50. Acevedo, JC; López, GV; Berbeo, ME; Zorro, O; Díaz, RC; Feo O. La drezotomía como tratamiento eficaz para el control del dolor neuropático de origen central por trauma raquimedular : caso clínico-evaluación a largo plazo. Univ med. 2013;54(2):268–81.
51. Petra, EM; Schothorst, M; Dallmeijer, A; Vermeulen, J; Van Ouwerkerk, W; Strijers, R; Becher J. Short- and long-term effects of selective dorsal rhizotomy on gross motor function in ambulatory children with spastic diplegia. J Neurosurg Pediatr. 2011;7(May):557–62.
52. Reynolds MR, Ray WZ, Strom RG, Blackburn SL, Lee A, Park TS. Clinical Outcomes After Selective Dorsal Rhizotomy in an Adult Population. WNEU [Internet]. 2010;75(1):138–44. Available from: http://dx.doi.org/10.1016/j.wneu.2010.09.010
53. Enslin JMN. The Evolution of Selective Dorsal Rhizotomy for the Management of Spasticity. Neurotherapeutics. 2019;16(3):3–8.
54. National Institute for Health and Clinical Excellence. Selective dorsal rhizotomy for spasticity in. NHS. 2010;(December).
55. Gump. WC; Mutchnick, MS; Miroarty T. Selective dorsal rhizotomy for spasticity not associated with cerebral palsy: reconsideration of surgical inclusion criteria. Neurosurg Focus. 2013;35(January 1980):1–6.
56. Park, TS; Johnston J. Surgical techniques of selective dorsal rhizotomy for spastic cerebral palsy. Neurosurg Focus. 2006;21(2):1–6.
57. Fukuhara T, Najm IM, Levin KH, Luciano MG, Ph D, Brant CL. Nerve Rootlets to Be Sectioned for Spasticity Resolution in Selective Dorsal Rhizotomy. Surg Neurol. 2000;54:126–33.
58. Mukherjee A, Chakravarty A. Spasticity mechanisms – for the clinician. Front Neurol. 2010;1(December):1–10.

This work is licensed under a Creative Commons Attribution 4.0 International License.